A 49-year-old man with unilateral, nontender left eyelid swelling
Digital Journal of Ophthalmology 2014
Volume 20, Number 1
January 17, 2014
DOI: 10.5693/djo.03.2013.09.007
Volume 20, Number 1
January 17, 2014
DOI: 10.5693/djo.03.2013.09.007
Download PDF
Past medical and surgical history were unremarkable. Other than the 2 previous eyelid lancings, the patient denied any other eyelid surgery, injectables, or ocular history. The patient was not on any medications. Family and social history were noncontributory.
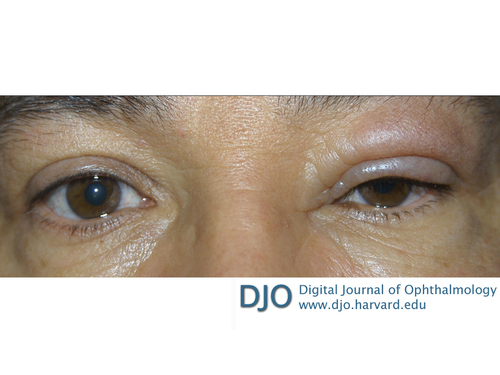
Figure 1
A 49-year-old man with left upper eyelid swelling of 14 months’ duration at presentation.
A 49-year-old man with left upper eyelid swelling of 14 months’ duration at presentation.
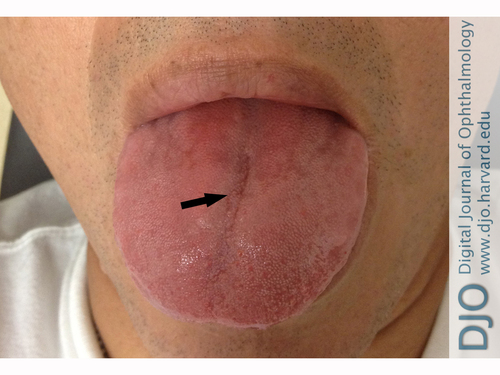
Figure 2
Patient at presentation with relatively normal tongue, with only a mild fissure located centrally (arrow).
Patient at presentation with relatively normal tongue, with only a mild fissure located centrally (arrow).
Eyelid infections, such as periorbital or orbital cellulitis, may present with eyelid edema. Periorbital infections are preseptal and can be caused by trauma, bacteremia, or upper respiratory illnesses. Patients experience eyelid induration, erythema, and tenderness. Orbital cellulitis involves the orbit itself; symptoms are severe, including proptosis, pain on eye movement, ophthalmoplegia with diplopia, and decreased visual acuity. A diagnosis of periorbital or orbital cellulitis can be made based on history and physical examination, although computed tomography or magnetic resonance imaging can be helpful in evaluating for orbital cellulitis and its complications.
Thyroid orbitopathy can cause chronic eyelid edema, although it is usually bilateral and occurs in older individuals (40-60 years of age). It is associated with lagophthalmos, eyelid retraction, and proptosis. It can be excluded by laboratory tests and orbital imaging studies.
Blepharochalasis can also present with eyelid edema that is usually bilateral, although it can occur unilaterally. It is characterized by recurrent episodes of nonpainful, nonerythematous upper eyelid swelling that usually begins in childhood or adolescence. These episodes last an average of 2 days, but recurrent episodes can cause the eyelids to become discolored, thin, and wrinkled, with the classic appearance of tissue paper. These episodes have been noted to decrease in frequency as patients age. Treatment is primary surgical and aims to restore function and maintain cosmesis.(1)
Angioedema can be hereditary or acquired. Hereditary angioedema can be detected with laboratory testing for C1 inhibitor protein and complement C4 levels. The acquired form is often caused by an immunologic response to an allergen and may occur with other allergy symptoms. Angioedema due to an allergen usually responds to treatment with antihistamines or steroids.
Lymphedema is usually the result of invasive surgical procedures that result in lymphoceles or lymph fistulas, which are most commonly described in vascular procedures involving the lower extremities. Lymphorrhea is usually a clear, amber-colored fluid unlike the dark fluid seen in our patient.
Allergic or contact dermatitis could also present with eyelid swelling. This hypersensitivity reaction can occur with a variety of allergens, and patients present with pruritus and inflammation at the affected site. A unilateral presentation would be uncommon, and our patient did not identify any unusual contacts to precipitate an allergic response. Diagnosis can be made clinically, with an emphasis on a detailed history, and is confirmed by patch testing.
Eyelid malignancies, periorbital pseudotumor, and eosinophilic granulomas may be diagnosed by biopsy. Patients with ocular rosacea may present with associated skin findings, including rhinophyma, pustules, papules, and erythema.
The MRI results, combined with a negative laboratory work-up for other possible causes of eyelid edema and questionable tongue abnormality, led to a diagnostic biopsy of the upper left eyelid. A full thickness biopsy, including skin and orbicularis oculi, was taken from the space between the lid crease and the brow, yielding a 3.5 × 1.0 × 0.1 cm tissue specimen. Histopathologic evaluation of the specimen showed diffuse edema of the superficial dermis accompanied by ectatic lymphatics and loosely formed, noncaseating granulomas, many of which appeared to be within the lumens of lymphatics or vessels (Figure 4). All stains, including Gram stain, and special stains for microorganisms (Periodic acid-Schiff and acid-fast bacilli) were negative, and no polarizable foreign material was identified. No eosinophils were noted. Immunohistochemical staining with D2-40 and CD68 confirmed the presence of ectatic lymphatics and intralymphatic histiocytosis. Based on the clinical symptoms, combined with the histopathologic results, a diagnosis of Melkersson-Rosenthal syndrome was made.
Melkersson-Rosenthal syndrome (MRS) is classically described as a triad of recurrent facial paralysis, orofacial edema, and fissuring of the tongue (lingua plicata).(2) The dominant feature of the syndrome is orofacial edema, which is painless, nonpitting, unilateral, and typically includes the eyelids and lips.(3) The facial paralysis can be unilateral (mimicking Bell’s palsy) or bilateral.(4) Lingua plicata is the rarest component of the triad and is not considered pathognomonic of the disease. Patients may be mono- or oligo-symptomatic, and in such cases the presence of only one or two features in the triad can make this a challenging diagnosis. Moreover, the features may present over a period of years, which further complicates the diagnosis.(5) The etiology of the syndrome remains unclear, though autoimmune or viral causes have been hypothesized.(3,6) Symptoms tend to present around the second or third decade of life, although infrequently they can present in childhood or after 50 years of age.(7) Studies regarding the gender predisposition for the syndrome are conflicting, with females being equally or slightly more affected than males.(3,8)
Our patient did not manifest the classic triad of Melkersson-Rosenthal syndrome, presenting only with isolated left upper eyelid edema and no clinical evidence of facial nerve paralysis or gross lingua plicata. A diagnosis of MRS requires a high index of clinical suspicion as well as histopathological evidence for confirmation of the diagnosis. The distinctive histopathology of MRS is described as non-caseating, granulomatous lymphangitis with granulomas within and around the lymphatics and blood.(3,4,8) MRS should be considered in patients presenting with eyelid edema of unknown etiology and biopsy should be performed.(9)
Initial treatment for Melkersson-Rosenthal syndrome usually consists of topical, intralesional, or systemic corticosteroid therapy, although the syndrome is often refractory to treatment. Patients with MRS are also treated with nonsteroidal, anti-inflammatory drugs such as metronidazole, dapsone, acyclovir, methotrexate, and thalidomide, with varying levels of response.(5) Clofazimine, an anti-lepromatous drug, has also been reported to decrease some of the eyelid swelling and associated granulomas.(10)
Surgical management of eyelid edema, such as debulking procedures or blepharoplasty, may be indicated if the edema is unresponsive to steroids, if it becomes visually significant, or becomes cosmetically unacceptable for the patient.(11)
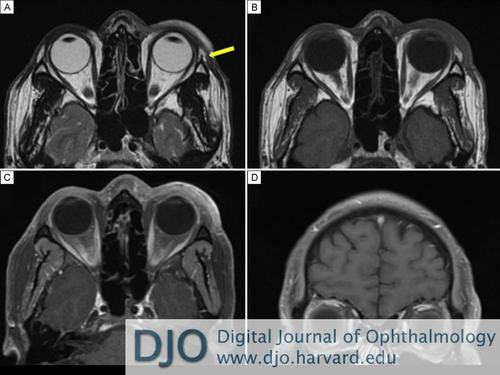
Figure 3
Magnetic resonance imaging of the orbits obtained in sequence. A, Axial T2-weighted imaging before contrast showing left eyelid tissue swelling and no evidence of lacrimal gland enlargement (yellow arrow). B, Axial T1-weighted imaging before contrast showing left eyelid soft tissue swelling. C, Axial T1-weighted imaging after contrast with fat suppression showing continued left eyelid soft tissue swelling and no focal areas of enhancement. D, Coronal T1-weighted imaging after contrast with fat suppression showing no extraorbital masses or abnormal enlargement of extraocular muscles.
Magnetic resonance imaging of the orbits obtained in sequence. A, Axial T2-weighted imaging before contrast showing left eyelid tissue swelling and no evidence of lacrimal gland enlargement (yellow arrow). B, Axial T1-weighted imaging before contrast showing left eyelid soft tissue swelling. C, Axial T1-weighted imaging after contrast with fat suppression showing continued left eyelid soft tissue swelling and no focal areas of enhancement. D, Coronal T1-weighted imaging after contrast with fat suppression showing no extraorbital masses or abnormal enlargement of extraocular muscles.
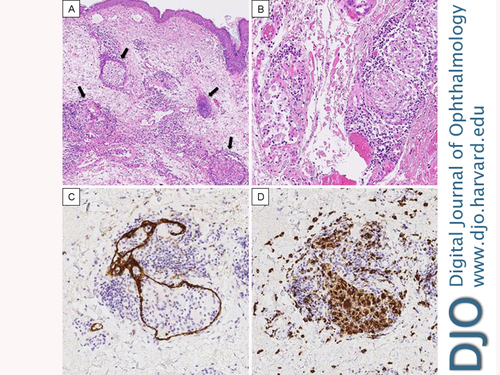
Figure 4
A, A low-power photomicrograph showing dermal edema, dilated lymphatics and noncaseating granulomas (black arrows) associated with the lymphovasculature along with an infiltrate of chronic inflammatory cells (hematoxylin and eosin, original magnification × 10). B, High-power image of the granulomas showing a loose collection of histiocytes possibly within the lumen of a lymphatic or vessel. Chronic inflammation is present surrounding the granulomas (hematoxylin and eosin, original magnification × 20). C, The D2-40 stain highlights the presence of a lymphatic wall surrounding a loosely formed granuloma. D, The presence of the intralymphatic granuloma is confirmed by the CD68 stain.
A, A low-power photomicrograph showing dermal edema, dilated lymphatics and noncaseating granulomas (black arrows) associated with the lymphovasculature along with an infiltrate of chronic inflammatory cells (hematoxylin and eosin, original magnification × 10). B, High-power image of the granulomas showing a loose collection of histiocytes possibly within the lumen of a lymphatic or vessel. Chronic inflammation is present surrounding the granulomas (hematoxylin and eosin, original magnification × 20). C, The D2-40 stain highlights the presence of a lymphatic wall surrounding a loosely formed granuloma. D, The presence of the intralymphatic granuloma is confirmed by the CD68 stain.
2. Talabi OA. Melkerssons-Rosenthal syndrome: a case report and review of the literature. Niger J Clin Pract 2011;14:477-8.
3. Cockerham KP, Hidayat AA, Cockerham GC, et al. Melkersson-Rosenthal syndrome: new clinicopathologic findings in 4 cases. Arch Ophthalmol 2000;118:227-32.
4. Akarsu C, Atasoy P, Erdogan S, Kocak M. Bilateral upper eyelid edema in Melkersson-Rosenthal syndrome. Ophthal Plast Reconstr Surg 2005;21:243-5.
5. Elias MK, Mateen FJ, Weiler CR. The Melkersson-Rosenthal syndrome: a retrospective study of biopsied cases. J Neurol 2013;260;138-43.
6. Giovannetti A, Mazzetta F, Cavani A, et al. Skewed T-cell receptor variable â repertoire and massive T-cell activation in idiopathic facial granulomatosis. Int J Immunopathol Pharmacol 2012;25:503-11.
7. Pierre-Filho Pde T, Rocha EM, Natalino R, Cintra ML, Caldato R. Upper eyelid oedema in Melkersson-Rosenthal syndrome. Clin Experiment Ophthalmol 2004;32:439-40.
8. Rawlings NG, Valenzuela AA, Allen LH, Heathcote JG. Isolated eyelid edema in Melkersson-Rosenthal syndrome: a case series. Eye (Lond) 2012;26:163-6.
9. Yeatts RP, White WL. Granulomatous blepharitis as a sign of Melkersson-Rosenthal syndrome. Ophthalmology 1997;104:1185-9;discussion 1189-90.
10. Podmore P, Burrows D. Clofazamine-an effective treatment for Melkersson-Rosenthal syndrome or Miescher’s cheilitis. Clin Exp Dermatol 1986;11:173-8.
11. Kondratiev S, Heher K, Baker BJ, Laver NV. Melkersson-Rosenthal syndrome presenting as chronic eyelid swelling. Ophthalmic Surg Lasers Imaging 2010;9:1-3.