A 5-year-old girl with left upper eyelid swelling
Digital Journal of Ophthalmology 2012
Volume 18, Number 4
December 31, 2012
DOI: 10.5693/djo.03.2012.05.001
Volume 18, Number 4
December 31, 2012
DOI: 10.5693/djo.03.2012.05.001
Download PDF

Figure 1
A 5-year-old girl with upper eyelid edema, at presentation.
A 5-year-old girl with upper eyelid edema, at presentation.
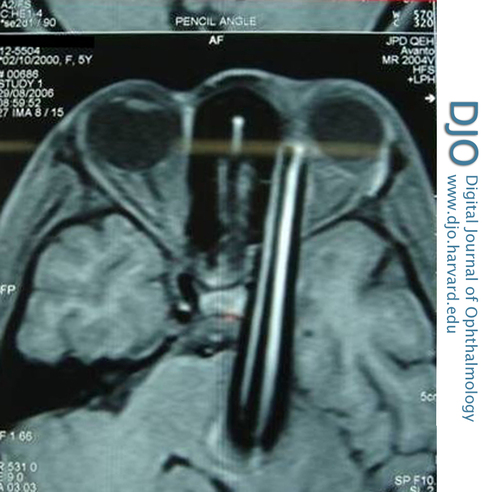
Figure 2
Magnetic resonance imaging showing the intraorbital foreign body extending to the brainstem.
Magnetic resonance imaging showing the intraorbital foreign body extending to the brainstem.
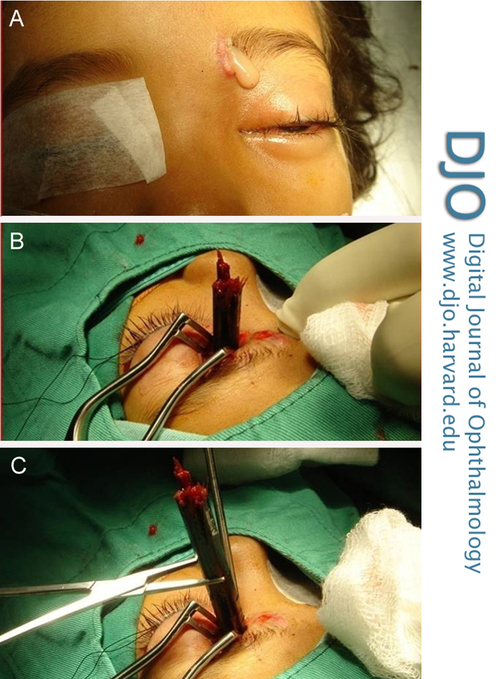
Figure 3
Three stages in the extraction of the foreign body.
Three stages in the extraction of the foreign body.

Figure 4
The pencil after extraction.
The pencil after extraction.
In civilian life, intraorbital foreign bodies are usually occupational in nature. Orbital roof fractures are also reportedly common. This is assumed to be due to the reflex extension of the patient’s head backward, exposing the orbital roof. The thin bony plate of the roof offers little resistance to the foreign body. However, the Wills Eye Institute study found the medial wall to be the most common site for foreign bodies to become lodged .(2)
It is important to assess the actual extent of injury so that appropriate management can be planned. Globe perforations and orbitocranial fractures are other injuries that must also be ruled out. The shocking feature seen in some cases of apparently trivial trauma is that patients may not be aware of any penetrating injury.(6) Occult foreign bodies which penetrate the orbit are only detected with secondary complications, including visual loss, severe orbital inflammation, meningitis, orbital cellulitis, osteomyelitis, ptosis, and brain abscess.(7-9)
Orbitocranial injuries can prove fatal. Death in a child from transhemispheric brain injury after intraorbital penetration with a pencil has been reported;(1) in another incident, a schizophrenic patient committed suicide by piercing his orbit with a plastic ballpoint pen, which entered the cerebellum.(10)
Orbitocranial injuries with foreign bodies can be silent at presentation. Thus even a minor injury should be assessed properly to rule-out severe comorbidities. These cases require imaging studies including CT and MRI; however, MRI should only be performed after a metallic foreign body has been ruled out. If vascular injury is suspected, angiography may be required.
Trauma to the cerebrovascular system (both penetrating and nonpenetrating) can cause injuries such as arterial dissection, pseudo-aneurysm, arterial or venous rupture or thrombosis, and arteriovenous fistula. A vascular injury should be suspected from frank hemorrhage or neurological deficits such as numbness, weakness, and paralysis of the face, upper or lower extremity, or entire side of the body. There may also be a loss of consciousness, facial drooping, slurred speech, aphasia, confusion, blurred vision, and impaired breathing or swallowing. Nausea and vomiting may also occur. If a vascular injury is detected on angiography, measures must be taken preoperatively to control any intraoperative bleeding.
Orbital injuries can lead to enophthalmos or proptosis, ecchymosis, restricted ocular movements, diplopia, chemosis, and crepitus. The presence of such symptoms and signs warrants detailed radiological investigations to assess the severity of the injury.
Resolution of orbitocranial penetrating injury usually requires a multidisciplinary approach, involving neurosurgical and vascular specialists; postoperatively psychiatric evaluation and counseling may be advisable. In children it is also essential to rule out abuse.
Removing a long foreign body through an anterior approach appears to be a simple procedure; however, there is a risk of orbital hemorrhage and lethal intracranial bleeding. Craniotomy and/or an endovascular approach needs to be performed for those presenting with symptoms of vascular involvement or if the foreign body has no extracranial extension. Such cases should be undertaken with neurosurgical and vascular surgical support.
In conclusion, a case of “trivial” eyelid trauma might be associated with a more serious occult problem. In cases involving children, where history taking can be especially challenging, a high index of suspicion, thorough evaluation of the patient, and proper imaging studies can prevent clinical catastrophes.
2. Shelsta HN, Bilyk JR, Penne, RE, Carrasco JR. Wooden intraorbital foreign body injuries: clinical characteristics and outcomes of 23 patients. Ophthal Plast Reconstr Surg 2010; 26: 238-44.
3. Elgin U, Berker N, Nalcaciouglu P, Ucan N. Nonsurgical management of an intraorbital pencil without cranial or globe penetration. J Pediatr Ophthalmol Strabismus 2007;44:307-8.
4. Ozer S, Onal B, Akbay A, Onerci M. Craniocerebral injury resulting from pencil penetration. Eur Arch Otorhinolaryngol 2010;267:155-7.
5. Shriwas SR, Kinzha AZ. Orbital injuries in children: Play-related. Ind J Ophth 1993;41;129-30.
6. Dinakaran S, Noble PJ. Silent orbitocranial penetration by a pencil. J Accid Emerg Med 1998;15:274-6.
7. Bursick DM, Selker RG. Intracranial pencil injuries. Surgical neurology 1981; 16; 427-31.
8. Horner FA, Berry RG, Frantz M. Broken pencil points as a cause of brain abscess. N Engl J Med 1964;271:342-5.
9. Seider N, Gilboa M, Lautman E, Miller B. Delayed presentation of orbito-cerebral abscess caused by pencil-tip injury. Ophthal Plast Reconstr Surg 2006;22:316-7.
10. Lunetta P, Öhberg A, Sajantila A. Suicide by intracerebellar ballpoint pen. Am J Forensic Med Pathol 2002;23:334-7.