A 64-year-old woman with dilated right pupil, nausea, and headache
Digital Journal of Ophthalmology 2013
Volume 19, Number 1
January 27, 2013
DOI: 10.5693/djo.03.2012.11.001
Volume 19, Number 1
January 27, 2013
DOI: 10.5693/djo.03.2012.11.001
Download PDF
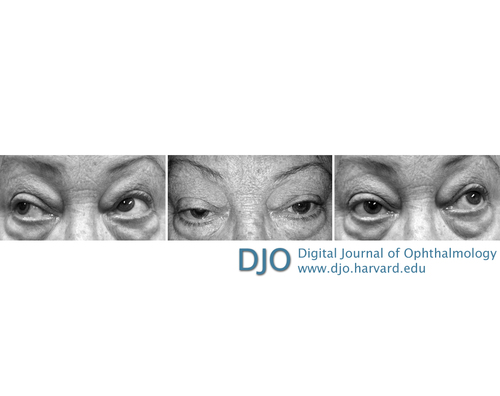
Figure 1
Photographs showing right oculomotor nerve palsy, with sparing of abducens nerve function (abduction) in right gaze, ptosis and mydriasis of the right eye in primary position, and restricted adduction in left gaze.
Photographs showing right oculomotor nerve palsy, with sparing of abducens nerve function (abduction) in right gaze, ptosis and mydriasis of the right eye in primary position, and restricted adduction in left gaze.
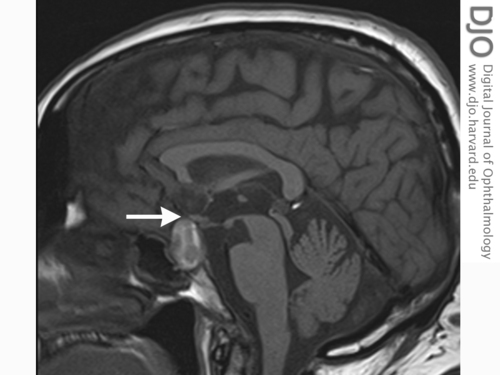
Figure 2
T1-weighted magnetic resonance imaging (MRI), sagittal view, showing hyperintense sellar mass (optic chiasm indicated by arrow).
T1-weighted magnetic resonance imaging (MRI), sagittal view, showing hyperintense sellar mass (optic chiasm indicated by arrow).
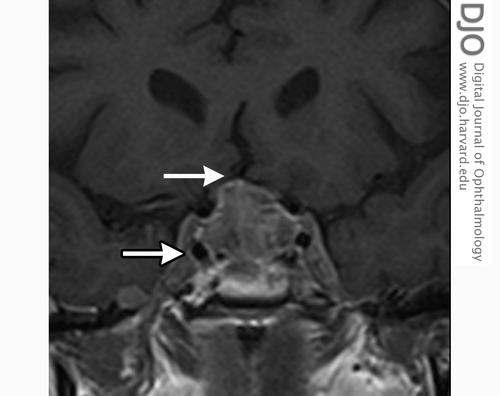
Figure 3
MRI, coronal view, showing gross expansion of pituitary fossa with heterogeneous high T1 signal reflecting blood products. There is infiltration of the cavernous sinuses (outlined arrow) bilaterally with effacement of the undersurface of the optic chiasm (arrow).
MRI, coronal view, showing gross expansion of pituitary fossa with heterogeneous high T1 signal reflecting blood products. There is infiltration of the cavernous sinuses (outlined arrow) bilaterally with effacement of the undersurface of the optic chiasm (arrow).
This patient presented with pupil-involving oculomotor nerve palsy. An important differential that must be considered with pupil involvement is an evolving compressive oculomotor nerve lesion. An urgent angiogram is needed to exclude an aneurysm.
Acute-onset paralysis of the oculomotor nerve has been described as the chief presenting complaint of pituitary apoplexy in only a few cases in the literature.(1) Pituitary apoplexy refers to the clinical syndrome associated with hemorrhagic infarction of a preexisting pituitary adenoma, classically manifesting with the sudden onset of headache, nausea and vomiting, visual impairment (decreased acuity, field deficits, or impaired ocular motility), and altered mental status. The word “apoplexy” is of Greek origin and describes the accumulation of blood or fluid within any organ.(1) Apoplectic events are unpredictable and often misdiagnosed.(2) The presentation may also be complicated by meningism. Delayed diagnosis increases the risk of permanent visual impairment. Successful management of pituitary apoplexy relies on early diagnosis, with appropriate medical management of acute adrenal insufficiency and surgical intervention to optimize visual outcome. The history may have clues to the longstanding presence of a pituitary tumor (headache, visual loss, endocrine problems), with the acute episode manifested by signs of compression by hematoma and pituitary destruction. Pituitary function tests, such as prolactin, thyroid function, and gonadotropins, are also essential to guide further hormonal therapy and confirm the extent of pituitary compromise.
A timely diagnosis of pituitary apoplexy of a preexisting pituitary adenoma was made in this case. Pituitary apoplexy is an uncommon and potentially fatal condition. It is a sight-threatening emergency for which a variety of presenting features have been described. Various degrees of cranial nerve palsy can result from compression of cranial nerves III, IV, V, and VI, with an expanding mass in the cavernous sinus.(5) However, isolated oculomotor nerve palsy without visual acuity or field deficits as the presenting sign of pituitary apoplexy is rare (Table 1).
In a retrospective series, Randeva et al found headache to be the most reliable presenting symptom, followed by nausea and a reduction in visual fields.(3) Additional symptoms include changes in the level of consciousness, meningeal irritation, and ophthalmoplegia.(1) The triad of incomplete eye movements, pupil asymmetry, and ptosis is suggestive of an oculomotor nerve lesion with pupillary dilatation in addition to ptosis being indicative of a mass lesion compressing the oculomotor nerve. Possible compression within the subarachnoid space should also be considered, as with a posterior-communicating arterial aneurysm or a supratentorial mass with impending herniation. Ophthalmic manifestations of pituitary apoplexy arise from superior and/or lateral expansion of the tumor.(6)
The pituitary gland lies in the sella turcica, near the hypothalamus and optic chiasm. It is surrounded by the sphenoid bone and covered by the sellar diaphragm (an extension of the dura). Like the cranial vault, the walls of the sella turcica are normally rigid with sudden and rapid rises in intrasellar pressure resulting from apoplexy. Visual field impairment is common with superior expansion into the optic nerve or chiasm from which a bitemporal defect is classically seen. Formal documentation of any field defects should be obtained at presentation in all stable patients.
The present case demonstrated radiological mass effect on the optic chiasm without any visual acuity or visual field deficits. Cases of oculomotor nerve palsy without visual field defects have been reported and follow a favorable prognosis (Table 1). Diplopia occurs due to compression of the cranial nerves in the cavernous sinus but may be masked by ptosis, obscuring vision in the affected eye in some cases of oculomotor nerve palsy.(7) The oculomotor nerve is the third and largest of the cranial nerves to the extraocular muscles and lies below the optic tract as it pierces the arachnoid and dura matter at the roof of the cavernous sinus. Possible mechanisms of oculomotor nerve palsy from pituitary adenomas include direct compression of the nerve by tumor invasion of the cavernous sinus, transmission of pressure on the cavernous sinus wall by tumor expansion, edematous expansion due to hemorrhage or ischemic infarction of the tumor, direct infiltration of the tumor, and vascular occlusion of the nerve (8). Because it is more horizontally situated in the cavernous sinus, the oculomotor nerve is susceptible to lateral pressure from an expanding mass compressing it between the tumor and the inter-clinoid ligament.(8,9) Despite being a commonly affected cranial nerve, cases of isolated oculomotor nerve palsy (without visual acuity or field deficits) are rarely described as the initial feature of ophthalmoplegia in pituitary apoplexy, perhaps because of the confluence of other structures within the cavernous sinus, making it unlikely for damage to the third nerve in this area to present as an isolated palsy.(10)
Although there are a few case series reported (8,11-13) of isolated oculomotor nerve palsy in pituitary apoplexy, most of these cases also included visual field and/or visual acuity deficits. In some cases, visual deficits were not mentioned or cases of isolated oculomotor nerve palsy were not elaborated and hence not included in our review.(8,11) To our knowledge, our study is the only compilation of isolated oculomotor nerve palsy case reports without visual deficits in the literature (Table 1). In total, there were 19 case reports (including the present case), of which the majority were non-functioning pituitary adenomas. In case number 11, there was no mention of treatment or the outcome.(14) Two cases each were of Cushing’s disease and prolactinomas. (9,14,15) In the majority of these cases, no precipitating factors were found. The precipitating factors include 2 cases of mild head injury (16) and 1 each of Sheehan’s syndrome (5) and anticoagulation (present case). In contrast, Sibal et al found that 40% of pituitary apoplexy cases had a precipitating factor.(12) In complete oculomotor nerve palsies, 5 of each were treated with surgery and conservative treatment, with complete recovery in all cases. (6,9,10,15-18) In incomplete paresis cases, 7 underwent surgery and 1 conservative treatment.(5,9,10,14,19,20) All recovered completely except for 1 case, in which the palsy had been present for 10 months.(9)
Our patient did not require surgery and recovered complete oculomotor nerve function within 3 days of steroid treatment. At follow-up at 1 and 2 months after discharge, sustained resolution of the palsy was noted; formal field testing, repeated after 3 months, was normal. Because there are no randomized trials on pituitary apoplexy cases with cranial neuropathy, there is no evidence in favor of either surgery or conservative treatment. Randeva et al reported improvement in ocular paresis with surgery, with complete recovery of visual acuity in all cases if operated within 8 days and complete recovery in 46% of cases if operated after 8 days. The present case, by contrast, describes isolated ophthalmoplegia without visual acuity or field deficits.(3) Kim et al noted that time to recovery from cranial nerve palsies accompanying pituitary tumors after surgery and the interval between development of symptoms and surgery were positively and significantly correlated.(8) Maccagnan et al and Gruber et al found no evidence that early operative decompression is associated with an improved outcome.(21,22) Most of the patients managed conservatively had minor visual field and acuity deficits. As indicated in our compilation, pure oculomotor palsies recover well with either conservative or surgical treatment.
The acute onset of isolated oculomotor nerve palsy with pupillary involvement should alert clinicians to the possibility of pituitary apoplexy and the need for urgent angiography to rule out an aneurysm, followed by MRI and early neurosurgical referral. Given the variability of presentation, the importance of recognizing a pituitary tumor as the etiology of isolated third nerve palsy has been emphasized. Pupillary involvement is a crucial diagnostic sign.
In conclusion, this case report emphasizes not only the importance of recognizing pituitary apoplexy as the etiology of isolated oculomotor nerve palsy but also the need for prompt imaging of the undifferentiated endocrine patient before commencing anticoagulation. Early ophthalmoplegia without visual field deficits may be monitored for spontaneous resolution of oculomotor nerve palsy. Conservative treatment can be successful in certain cases of pituitary apoplexy with oculomotor nerve involvement.
Literature Search
A systematic review of the English literature was conducted in 2011 on multiple databases (MEDLINE, PubMed, and EMBASE) for relevant articles from the period 1950-2011. Search terms included pituitary apoplexy, isolated third nerve palsy, oculomotor, and anticoagulation. Only articles documenting isolated oculomotor nerve palsies without visual acuity or field deficits were compiled.
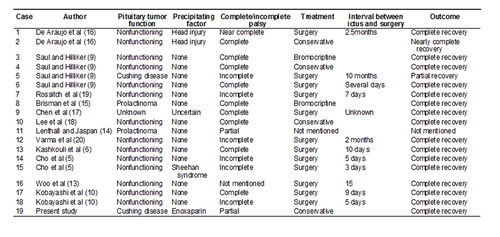
Table 1
Case report compilation of isolated oculomotor nerve palsies without documented visual field or acuity deficits
Case report compilation of isolated oculomotor nerve palsies without documented visual field or acuity deficits
2. Biousse V, Newman NJ, Oyesiku NM. Precipitating factors in pituitary apoplexy. J Neurol Neurosurg Psychiatry 2001;71:542- 545
3. Randeva HS, Schoebel J, Byrne J, et al. Classical pituitary apoplexy: clinical features, management and outcome. Clin Endocrinol 1999;51:181-8.
4. Harris SM, Cannon JE, Carroll PV, Thomas SM. Pituitary apoplexy: two very different presentations with one unifying diagnosis. J R Soc Med Sh Rep 2010;1:53.
5. Cho W, Joo S, Kim T, Seo B. Pituitary apoplexy presenting as isolated third cranial nerve palsy with ptosis: two case reports. J Korean Neurosurg Soc 2009;45:118-21.
6. Kashkouli MB, Khalatbari M, Yahyavi S, et al. Pituitary apoplexy presenting as acute painful isolated unilateral third cranial nerve palsy. Arch Iranian Med 2008;11:466-8.
7. Sowka JW, Gurwood AS, Kabat AG. Neuro-ophthalmic disease: Cranial nerve III palsy. Review of Optometry: The Handbook of Ocular Disease Management, 11th ed. April 15, 2009:50A-52A.
8. Kim SH, Lee KC, Kim SH. Cranial nerve palsies accompanying pituitary tumour. J Clin Neurosci 2007;14:1158-62.
9. Saul RF, Hilliker JK. Third nerve palsy: the presenting sign of a pituitary adenoma in five patients and the only neurological sign in four patients. J Clin Neuroophthalmol 1985;5:185-93.
10. Kobayashi et al. A possible mechanism of isolated oculomotor nerve palsy by apoplexy of pituitary adenoma without cavernous sinus invasion: a report of two cases. Acta Neurochir 2011;153:2453-6.
11. Dubuisson AS, Beckers A, Stevenaert A. Classical pituitary tumour apoplexy: clinical features, management and outcomes in a series of 24 patients. Clin Neurol Neurosurg 2007;109:63-70.
12. Sibal L, Ball SG, Connolly V, et al. Pituitary apoplexy: a review of clinical presentation, management and outcome in 45 cases. Pituitary 2004;7:157-63.
13. Woo HJ, Hwang JH, Hwang SK, Park YM. Clinical outcome of cranial neuropathy in patients with pituitary apoplexy. J Korean Neurosurg Soc 2010;48:213-8.
14. Lethall RK, Jaspan T. A case of isolated third nerve palsy with pupil involvement. Br J Radiol 2000;73:569-70.
15. Brisman M H Katz, Post KD. Symptoms of pituitary apoplexy rapidly reversed with bromocriptine. J Neurosurg 1996;85:1153-5.
16. De Araujo L C, Zapupulla RA, Quinonez R O, Noh J M. Pituitary adenoma presenting as post-traumatic oculomotor palsy: report of two cases. Neurosurgery 1979;4:427-30.
17. Chen HY, Tsai RK, Howng SL. Acute painful oculomotor nerve paresis caused by pituitary apoplexy—a case report. Kaohsiung J Med Sci 1999;15:437-40.
18. Lee C C, Cho A S, Carter W A. Emergency department presentation of pituitary apoplexy. Am J Emerg Med 2000;18:328-31.
19. Rossitch E, Carrazana E J, Black PM. Isolated oculomotor nerve palsy following apoplexy of a pituitary adenoma. J Neurosurg Sci 1992;103-5.
20. Varma D, Tesha P, George N. Acute painful third nerve palsy: the sole presenting sign of a pituitary adenoma. Eye 2002;16:792-3.
21. Maccagnan P, Macedo CL, Kayath MJ, et al. Conservative management of pituitary apoplexy: a prospective study. J Clin Endocrinol Metab 1995;80:2190-7.
22. Gruber A, Clayton J, Kumar S, et al. Pituitary apoplexy: retrospective review of 30 patients—is surgical intervention always necessary? Br J Neurosurg 2006;20:379-85.