A 31-year-old man with vitritis, chorioretinitis, and hydrocephalus
Digital Journal of Ophthalmology 2012
Volume 18, Number 2
May 14, 2012
DOI: 10.5693/djo.03.2012.03.001
Volume 18, Number 2
May 14, 2012
DOI: 10.5693/djo.03.2012.03.001
Download PDF
The patient was in his usual state of excellent health preceding the episode. He reported mild pressure in the affected eye along with a constant, bilateral, temporal headache that may have predated the blurred vision. The headache was readily relieved by acetaminophen. He denied flashes, photosensitivity, or other visual aberrations. He maintained that his vision was "weaker" on the right at baseline. On further questioning, he felt that his symptom was best characterized as "many floaters" in the right eye. He believed he may have been exposed to a toxic chemical at his workplace 2 months prior to this presentation.
The patient’s past medical history was unremarkable. He had no known drug allergies, and he denied a family history of medical or surgical conditions. His social history was significant for the use of occasional alcohol. He denied high-risk sexual activities, intravenous drug use, and blood transfusions.
Dilated stereoscopic fundus examination revealed 2+ vitreous cell in the right eye and bilateral optic nerve head edema (Figures 1-2). Indirect ophthalmoscopy of the right eye demonstrated a large, pigmented, inferotemporal chorioretinal scar with a superjacent area of presumed retinitis (Figure 3). The macula and peripheral retina of the left eye were normal.

Figure 1
Right fundus, optic nerve head margins appear blurred. Details obscured due to vitritis.
Right fundus, optic nerve head margins appear blurred. Details obscured due to vitritis.

Figure 2
Right fundus, centered on chorioretinal lesion inferotemporal to macula. The lesion is notable for encircling pigment and the suggestion of retinitis at superior border (denoted by arrow).
Right fundus, centered on chorioretinal lesion inferotemporal to macula. The lesion is notable for encircling pigment and the suggestion of retinitis at superior border (denoted by arrow).
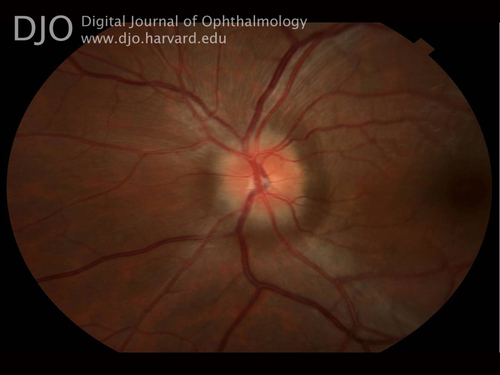
Figure 3
Left fundus showing optic disc edema.
Left fundus showing optic disc edema.
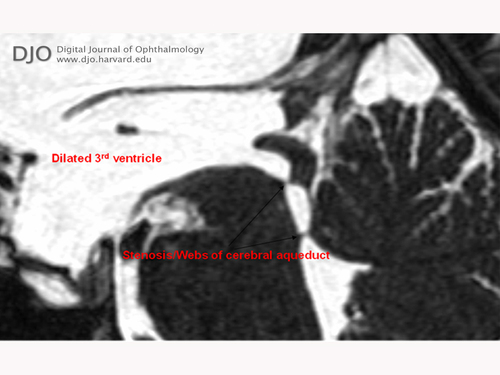
Figure 5
MRI, T2 FIESTA protocol, sagittal view, delineating anatomy of ventricles and CSF flow.
MRI, T2 FIESTA protocol, sagittal view, delineating anatomy of ventricles and CSF flow.

Figure 6
MRI FIESTA, coronal view, revealing engorgement of the lateral and 3rd ventricles.
MRI FIESTA, coronal view, revealing engorgement of the lateral and 3rd ventricles.

Figure 4
CT brain without contrast, axial view, revealing symmetric enlargement of the lateral ventricles.
CT brain without contrast, axial view, revealing symmetric enlargement of the lateral ventricles.
Classically, congenital toxoplasmosis is characterized by the triad of hydrocephalus, chorioretinal lesions, and cerebral calcifications.(1) Chorioretinal involvement is present up to 85% of infected subjects before adulthood.(2) In two large, retrospective, population-based studies, 28% to 50% of children diagnosed with congenital toxoplasmosis were found to have hydrocephalus.(3)
Cerebral toxoplasmosis is considered to be the most common opportunistic infection affecting the central nervous system in patients with HIV/AIDS.(4) However, hydrocephalus in the setting of cerebral toxoplasmosis without an associated mass lesion is an extremely rare; it has been described in fewer than 5 case reports.(5)
Though we cannot directly determine the chronicity of our patient’s conditions, it is possible that his hydrocephalus was longstanding based on the relatively normal intracranial pressure (16 cm fluid height) obtained upon fenestration of the 3rd ventricle by the neurosurgical team—a so-called “compensated” hydrocephalus. His discs, however, lacked the hallmarks of swelling secondary to chronic ICP elevation, including gliosis of the nerve fiber layer and optociliary shunt vessels. The symptoms of visual decline and headaches were also newly realized by the patient, suggesting at least an acute-on-chronic course.
Our patient initially had a good outcome with a shunting procedure, including resolution of his headache and subjective improvement in his vision. Unfortunately, serologic testing for toxoplasmosis was not obtained prior to his discharge, and he did not return to our service for follow-up. His particular presentation was suggestive of a unifying diagnosis: the cerebral and retinal stigmata of congenital toxoplasmosis. However, it is impossible to confirm this diagnosis without serologic evidence and further surveillance of the course of the disease.
2. Vasconcelos-Santos DV, Machado Azevedo DO, Campos WR, et al; Congenital Toxoplasmosis Brazilian Group. Congenital toxoplasmosis in southeastern Brazil: results of early ophthalmologic examination of a large cohort of neonates. Ophthalmology 2009 ;116:2199-205.e1.
3. McAuley J, Boyer KM, Patel D, et al. Early and longitudinal evaluations of treated infants and children and untreated historical patients with congenital toxoplasmosis: the Chicago Collaborative Treatment Trial. Clin Infect Dis 1994;18:38-72.
4. Cota GF, Assad EC, Christo PP, Giannetti AV, Santos Filho JA, Xavier MA. Ventriculitis: a rare case of primary cerebral toxoplasmosis in AIDS patient and literature review. Braz J Infect Dis 2008;12:101-4.
5. Nolla-Salas J, Ricart C, D’Olhaberriague L, et al. Hydrocephalus: an unusual CT presentation of cerebral toxoplasmosis in a patient with acquired immunodeficiency syndrome. Eur Neurol 1987;27:130-2.