A 44-year-old woman with a 3-month history of bilateral, painless visual loss in the absence of other symptoms
Digital Journal of Ophthalmology 2012
Volume 18, Number 4
December 31, 2012
DOI: 10.5693/djo.03.2012.12.001
Volume 18, Number 4
December 31, 2012
DOI: 10.5693/djo.03.2012.12.001
Download PDF
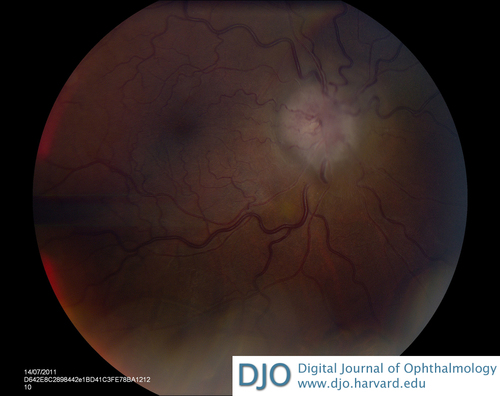
Figure 1
Papilledema of the right optic disc.
Papilledema of the right optic disc.
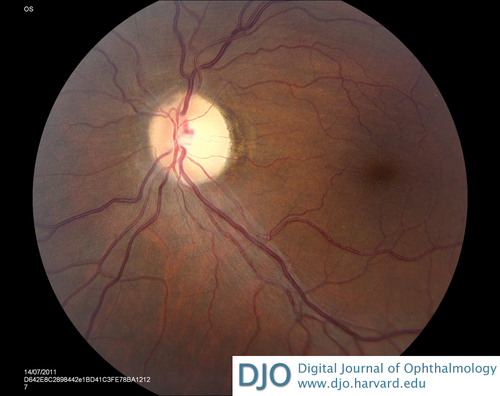
Figure 2
Left optic disc pallor.
Left optic disc pallor.
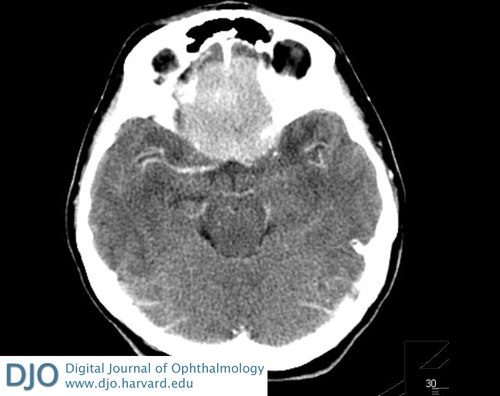
Figure 3
Computed tomography (CT) of the head showing a well-circumscribed homogenous lesion (4.6 × 4.4 × 2.5 cm) in the midline of the frontal region with surrounding edema consistent with meningioma.
Computed tomography (CT) of the head showing a well-circumscribed homogenous lesion (4.6 × 4.4 × 2.5 cm) in the midline of the frontal region with surrounding edema consistent with meningioma.
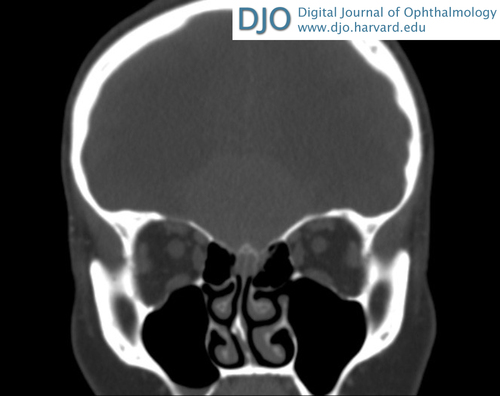
Figure 4
CT of the orbits showing no abnormality involving the globes, optic nerves, extraocular muscles, or any intraconal structures in either orbit; an intracranial mass is seen in the frontal region consistent with meningioma in the coronal view.
CT of the orbits showing no abnormality involving the globes, optic nerves, extraocular muscles, or any intraconal structures in either orbit; an intracranial mass is seen in the frontal region consistent with meningioma in the coronal view.
Foster Kennedy syndrome (FKS) consists of a clinical triad of optic atrophy in one eye, papilledema in the contralateral eye, and anosmia, caused by space-occupying anterior fossa masses.(1) Associated symptoms of raised intracranial pressure, including nausea, vomiting, and headaches, and frontal lobe signs may be present, including emotional lability and memory loss.
In pseudo-FKS, optic disc pallor and contralateral disc swelling is present but is not caused by an intracranial mass. This may be caused by the same pathological process in each eye. For example, patients with bilateral sequential ischemic optic neuropathy or optic neuritis may have one pale, atrophic optic disc and a papillitis in the contralateral optic disc, mimicking the papilledema seen in FKS. Alternatively, two pathological processes may be responsible: any cause of unilateral optic disc pallor (eg, previous unilateral ischemic optic neuropathy or optic neuritis; unilateral optic nerve hypoplasia) in conjunction with raised intracranial pressure causing papilledema in the contralateral eye will give rise to this combination of signs.(2) Papilledema does not occur in optic atrophy because the loss of neural fibers in optic atrophy results in a lack of neurons to swell.
FKS may present with a relative afferent pupillary defect early on if one optic nerve is predominantly affected. Chronic papilledema may lead to nerve fiber atrophy, a degree of which may already have existed in our patient, which would explain the absence of relative afferent pupillary defect on examination. As in any cause of optic nerve dysfunction, reduced color vision is an early feature. Visual field defects, including a central scotoma, are typically present. In patients presenting with decreased visual acuity, testing of color vision and pupillary reflexes should be performed in addition to fundus examination. The clinical signs of FKS may be readily apparent in cases of gross optic disc swelling or pallor; however, optic disc pallor may be extremely subtle and easily missed.
Poorly understood, with a currently debated pathogenesis and often insidious onset, FKS remains a diagnostic challenge. Early diagnosis, with subsequent surgical resection may prevent further visual deterioration and may allow some recovery of vision in these patients.(6) Disease awareness with early intracranial imaging and surgery is necessary to minimize the disabling sequelae of FKS.
2. Limaye SR, Adler J. Pseudo-Foster Kennedy syndrome in a patient with anterior ischemic optic neuropathy and a nonbasal glioma. J Clin Neuroophthalmol 1990;10:188-92.
3. Ruben S, Elston J, Hayward R. Pituitary adenoma presenting as the Foster-Kennedy syndrome. Br J Ophthalmology 1992;76:117-9.
4. Watnick RL, Trobe JD; Bilateral optic nerve compression as a mechanism for the Foster Kennedy syndrome. Ophthalmology 1989;96:1793-8.
5. Chamberlain MC, Blumenthal DT, Intracranial meningiomas: diagnosis and treatment. Expert Rev Neurother 2004;4:641-8.
6. Bulters DO, Shenouda E, Evans BT, Mathad N, Lang DA. Visual recovery following optic nerve decompression for chronic compressive neuropathy. Acta Neurochir (Wien). 2009;151:32.