A 39-year-old woman with unilateral metamorphosias
Digital Journal of Ophthalmology 2011
Volume 17, Number 4
November 20, 2011
DOI: 10.5693/djo.03.2011.11.001
Volume 17, Number 4
November 20, 2011
DOI: 10.5693/djo.03.2011.11.001
Download PDF
Dilated fundus examination of the left eye showed multiple, round, yellow lesions with ill-defined margins in the posterior pole; there was a larger one, slightly elevated, inferior to the fovea associated with a small retinal hemorrhage (Figure 1A). No vitreous cells were detected. Examination of the right eye was normal.
Indocyanine green angiography showed several areas of hypofluorescence in the right eye (Figure 1D), which corresponded to the visible subretinal lesions observed during fundus examination; the juxtafoveal lesion was hyperfluorescent, which confirmed the activity of the neovascular membrane.
Time-domain optical coherence tomography revealed a macular thickness of 246 µm in the left eye; there was no subretinal fluid (Figure 1E).
A complete work-up, including chest X-ray, serology for syphilis, immunoglobulins (IgM and IgG) for Toxoplasma and Borrelia burgdorferi and angiotensin-converting enzyme levels, was normal.
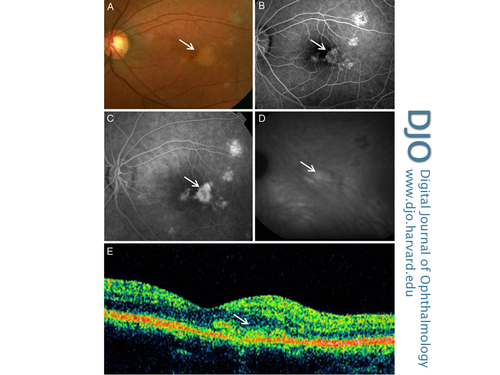
Figure 1
Left eye of patient with juxtafoveal choroidal neovascularization (arrows) secondary to punctate inner choroidopathy. A, Fundus photograph. B, Fluorescein angiogram showing early phase hyperfluorescence. C, Fluorescein angiogram showing midvenous phase hyperfluorescence. D, Indocyanine green angiogram showing areas of hyperfluorescence. E, Optical coherence tomography (OCT).
Left eye of patient with juxtafoveal choroidal neovascularization (arrows) secondary to punctate inner choroidopathy. A, Fundus photograph. B, Fluorescein angiogram showing early phase hyperfluorescence. C, Fluorescein angiogram showing midvenous phase hyperfluorescence. D, Indocyanine green angiogram showing areas of hyperfluorescence. E, Optical coherence tomography (OCT).
Four months after presentation, her visual acuity had improved to 1.0 and the metamorphopsias had resolved. Fluorescein angiography showed resolution of the choroidal neovascular lesion and complete resolution of the hemorrhage (Figure 2). Fluorescein angiography at 18 months' follow-up showed no recurrence of the choroidal neovascular membrane and her vision remained stable. No systemic or ocular adverse events were noted.
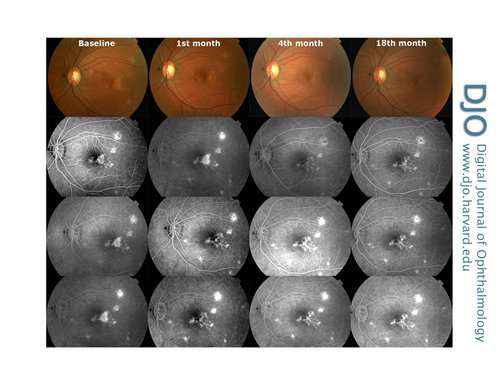
Figure 2
Fundus photographs and fluorescein angiograms of left eye before and 1, 4, and 18 months after intravitreal ranibizumab injections showing resolution of the hemorrhage and the choroidal neovascular membrane. The pretreatment fundus photograph shows a juxtafoveal choroidal neovascular membrane with multiple small chorioretinal lesions. Early and late phases of fluorescein angiogram showed window defects with no evidence of leakage.
Fundus photographs and fluorescein angiograms of left eye before and 1, 4, and 18 months after intravitreal ranibizumab injections showing resolution of the hemorrhage and the choroidal neovascular membrane. The pretreatment fundus photograph shows a juxtafoveal choroidal neovascular membrane with multiple small chorioretinal lesions. Early and late phases of fluorescein angiogram showed window defects with no evidence of leakage.
Inflammatory chorioretinopathies are often difficult to differentiate. Punctate inner choroidopathy (PIC), multifocal choroiditis and panuveitis (MCP), and presumed ocular histoplasmosis syndrome (POHS) are the subtypes most frequently associated with choroidal neovascularization; however, any other form of posterior uveitis, for instance, acute posterior multifocal placoid pigment epitheliopathy, birdshot retinochoroidopathy, multiple evanescent white dot syndrome, Vogt-Koyanagi-Harada syndrome, and sympathetic ophthalmia, can be complicated by choroidal neovascularization.(1)
PIC is an idiopathic inflammatory disorder that typically occurs in young (15-55 years), white, myopic women. Presenting symptoms are blurred vision and scotomas with or without flashes of light.(2) The symptoms are usually unilateral, but most patients show bilateral fundus involvement.(2,3) PIC is characterized by multifocal choroidal lesions (yellow-white lesions of the inner choroid and retinal pigment epithelium of approximately 100–300 ìm in size), usually distributed throughout the posterior pole but sparing the peripapillary region.(2,4) There are no other signs of ocular inflammation elsewhere in the eye. Visual prognosis is generally good since the lesions usually evolve into atrophic scars; however, choroidal neovascularization may develop in 17% to 40% of patients, potentially threatening central vision if untreated.(4-7)
MCP is an inflammatory disease that occurs in healthy young patients in their fourth decade, predominantly in white women. MCP is characterized by the presence of multiple small, yellow-gray choroidal lesions that, as the disease becomes inactive, are replaced by well-demarcated chorioretinal scars.(4) Patients with MCP typically have inflammatory cells in the anterior chamber or vitreous cavity at the time of presentation.(1) MCP may be complicated by choroidal neovascularization in 32% to 46% of the patients.(1) Choroidal neovascularization can occur more frequently in inflamed areas, although it may originate from an old chorioretinal scar.(4)
POHS is a bilateral immune reaction to an infectious agent, Histoplasma capsulatum, that affects the choroid and retina. It usually occurs in young patients. Men and women are equally affected. POHS is characterized by discrete atrophic choroidal scars in the macula and midperiphery associated with peripapillary atrophy and choroidal neovascularization—the classical triad of this disease (1). This triad is accompanied by complete absence of any signs of anterior chamber or vitreal inflammation. Choroidal neovascularization is associated with inactive choroidal scars (“histo-spots”); they do not demonstrate active inflammation.(1,4) The primary cause of visual impairment in POHS is the occurrence of choroidal neovascularization in the macula, which results in exudation and subsequent scarring.
Management of PIC-related choroidal neovascular membrane is a diagnostic and therapeutic challenge. In a minority of the cases, the choroidal neovascular membrane resolved spontaneously(3); however, the problem could worsen since the pathology is often bilateral and usually occurs in young active patients. Due to the rarity of these cases, our current understanding of PIC comes from relatively small case series, and there is a paucity of evidence on which to base the treatment strategies.
Multiple therapeutic strategies have been used, with varying success, including corticosteroids (8-10) interferon ß-1a,(11) subretinal surgery,(12) photodynamic therapy,(13) and, more recently, anti–vascular endothelial growth factor (anti-VEGF).(7,14-16)
Essex et al, in the largest series of patients diagnosed with PIC, reported a total of 153 eyes of 117 patients with PIC-related choroidal neovascular membranes; 26% of those eyes had a final visual acuity of less than 1/10.(2) The final outcome was similar in all groups with choroidal neovascular membrane, regardless of the treatment; however, in this series none of the patients were treated with anti-VEGF agents.
While clinical observations suggest that intravitreal anti-VEGF drugs are effective, the optimal number and frequency of intravitreal injections remains uncertain. Chan et al reported all 4 patients with PIC treated with 3 bevacizumab injections had visual improvement of at least 1 line.(14) According to a report by Kramer et al, a single injection of bevacizumab led to a rapid and lasting resolution of the choroidal neovascularization in a patient with PIC.(16) Menezo et al reported 9 of 10 patients having benefited from a mean of 1.9 injections of ranibizumab per eye.(7) Cornish et al reported 9 eyes with PIC-related choroidal neovascular membrane that responded to anti-VEGF treatment, with a mean of 2.34 injections per year.(17) In this series, there was a reduction of the subretinal fluid on OCT and a visual gain of 0.23 logMAR units.
In our patient, 2 injections of intravitreal ranibizumab resulted in complete and long-lasting visual and anatomic improvement in an eye with diagnosis of PIC-related choroidal neovascular membrane. The present case report supports the effectiveness of intravitreal antiangiogenic drugs as a primary treatment of PIC-related choroidal neovascular membrane; however, long-term follow-up is needed since there is a risk of recurrence of the choroidal neovascular membrane. Further prospective controlled studies and additional data are needed to establish the visual benefit, the long-term safety, and the optimal efficacy regimen of ranibizumab for PIC-related choroidal neovascular membrane.
2. Essex R, Wong J, Fraser-Bell S, Sandbach J, Tufail A, Bird A, Dowler J. Punctate inner choroidopathy. Arch of Ophthalmol 2010;128:982-7.
3. Watzke R, Packer A, Folk J, Benson W, Burgess D, Ober R. Punctate inner choroidopathy. Am J Ophthalmol 1984;98:572-84.
4. Amer R, Lois N. Punctate inner choroidopathy. Surv Ophthalmol 2011;56:36-53.
5. Gerstenblith A, Thorne J, Sobrin L, Do D, Shah S, Foster S, Jacobs D, Nguyen Q. Punctate inner choroidopathy: a survey analysis of 77 persons. Ophthalmology 2007;114:1201-4.
6. Brown J, Folk J, Reddy C, Kimura A. Visual prognosis of multifocal choroiditis, punctate inner choroidopathy, and the diffuse subretinal fibrosis syndrome Ophthalmol 1996;103:1100-5.
7. Menezo V, Cuthbertson F, Susan D. Positive response to intravitreal ranibizumab in the treatment of choroidal neovascularization secondary to punctate inner choroidopathy. Retina 2010;30. [Epub ahead of print]
8. Brueggeman R, Noffke A, Jampol L. Resolution of punctuate inner choroidopathy lesions with oral prednisone therapy. Arch Ophthalmol 2002; 120:996.
9. Levy J, Shneck M, Klemperer I, Lifshitz T. Punctate inner choroidopathy: resolution after oral steroid treatment and review of the literature. Can J Ophthalmol 2005;40:605-8.
10. Sim D, Sheth H, Kaines A, Tufail A. Punctate inner choroidopathy-associated choroidal neovascular membranes during pregnancy. Eye 2008;22:725-7.
11. Cirino A, Mathura J, Jampol L. Resolution of activity (choroiditis and choroidal neovascularization) of chronic recurrent punctate inner choroidopathy after treatment with interferon ß-1A. Retina 2006;26:1091-2.
12. Olsen TW, Capone A Jr, Sternberg P Jr, Grossniklaus HE, Martin DF, Aaberg TM Sr. Subfoveal choroidal neovascularization in punctate inner choroidopathy. Surgical managment and pathological findings. Ophthalmol 1996;103:2061-9.
13. Chatterjee S, Gibson J. Photodynamic therapy: a treatment option in choroidal neovascularisation secondary to punctate inner choroidopathy. Br J Ophthalmol 2003;87:925-7.
14. Chan WM, Lai T, Liu D, Lam D. Intravitreal Bevacizumab (Avastin) for choroidal neovascularization secondary to central serous chorioretinopathy, secondary to punctate inner choroidopathy or of idiopathic origin. Am J Ophthalmol 2007; 143: 977-83.
15. Vossmerbaeumer U, Spandau U, Baltz S, Wickenhaeuser A, Jonas J. Intravitreal bevacizumab for choroidal neovascularisation secondary to punctate inner choroidopathy. Clin Experiment Ophthalmol 2008;36:292-4.
16. Kramer M, Axer-Siegel R, Jaouni T, Reich E, Hemo I, Priel E, Averbukh E, Ehrlich R, Chowers I, Weinberger D, Amer R. Bevacizumab for choroidal neovascularization related to inflammatory diseases. Retina 2010;30:938-44.
17. Spiteri Cornish K, William GJ, Gavin MP, Imrie FR. Visual and optical coherence tomography outcomes of intravitreal bevacizumab and ranibizumab in inflammatory choroidal neovascularization secondary to punctuate inner choroidopathy. Eur J Ophthalmol 2011; 21:440-5.