A 16-year-old girl with bilateral optic disc swelling
Digital Journal of Ophthalmology 2011
Volume 17, Number 1
March 12, 2011
DOI: 10.5693/djo.03.2011.02.003
Volume 17, Number 1
March 12, 2011
DOI: 10.5693/djo.03.2011.02.003
Download PDF
According to her mother, she had gained about 10 kg in the previous 6 months. Her menstrual cycles were largely regular; she had neither dysmenorrhea nor menorrhagia. She presented to the hospital emergency department 7 months previously with right iliac fossa pain, which was attributed to constipation. She was discharged following dietary advice and laxatives, which relieved her symptoms.
General physical examination was normal, apart from a distended abdomen. At 76 kg, the patient was slightly overweight for her height (5'4") and her blood pressure was elevated, at 150/106 mm Hg. A pediatric referral was arranged. Ambulatory blood pressure monitoring by the pediatricians showed an average blood pressure of 156/110. A hypertensive work-up ensued.
Figure 1
Fundus photographs of right (A) and left (B) eyes at presentation.
Fundus photographs of right (A) and left (B) eyes at presentation.
Figure 2
Results of Goldmann visual field testing of right (A) and left (B) eyes at presentation.
Results of Goldmann visual field testing of right (A) and left (B) eyes at presentation.
A lumbar puncture showed clear and colorless cerebrospinal fluid, total protein count of 23 mg/100 mL (normal, 15-60 mg/100 mL), gamma globulin 11% of the total protein (normal, 3%-12% of total protein), glucose level of 76 mg/100 mL (normal, 50-80 mg/100mL), cell count of 0-5 white blood (all mononuclear) cells (normal, 0-5) with no red blood cells, and chloride level of 117 mEq/L (normal, 116-130 mEq/L). Microbiology of the cerebrospinal fluid was unremarkable, with no growth.
An electrocardiogram was normal.
In view of the normal lab work-up, an ultrasound of the abdomen was requested to rule out gynecological or renal causes of hypertension. Ultrasonography of the abdomen showed a large abdominal cyst extending from the symphysis pubis to the level of xyphisternum (Figure 3). Magnetic resonance imaging of the abdomen showed a cyst arising from the pelvis and measuring 34 × 29 × 12 cm. Within its right side border an additional septated area was seen, suggesting a small additional follicular cyst within a large ovarian cyst. No renal compression or hydronephrosis was noted.
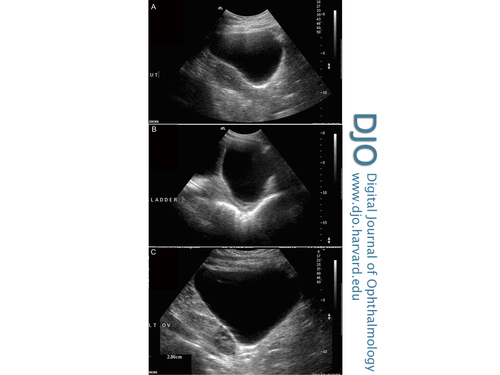
Figure 3
Ultrasonography of the abdomen showing a large abdominal cyst extending from symphysis pubis to the level of xyphisternum, approximately 25 cm in trasnsverse, 40-60 cm in longest axis and 20 cm deep (all at deepest and widest points): in relation to the uterus (UT) (A), the bladder (LADDER) (B), and the left ovary (LT OV) (C). Content is generally clear and anechoic, with a suggestion of a trace of debris at its dependant aspect.
Ultrasonography of the abdomen showing a large abdominal cyst extending from symphysis pubis to the level of xyphisternum, approximately 25 cm in trasnsverse, 40-60 cm in longest axis and 20 cm deep (all at deepest and widest points): in relation to the uterus (UT) (A), the bladder (LADDER) (B), and the left ovary (LT OV) (C). Content is generally clear and anechoic, with a suggestion of a trace of debris at its dependant aspect.
Figure 4
Results of Goldmann visual field testing of right eye (A) and left eye (B) after removal of cyst.
Results of Goldmann visual field testing of right eye (A) and left eye (B) after removal of cyst.
In hypertensive optic neuropathy, the mechanism of disc swelling is controversial, but ischemia of the optic nerve head is thought to play a role.(3) However, it is usually unilateral or, if bilateral, is frequently associated with other signs of hypertensive retinopathy, such as retinal hemorrhages and exudates and cotton wool spots. There can also be signs of hypertensive choroidopathy with exudative retinal detachments.(4)
Optic nerve head drusen can cause bilateral optic disc swelling, but spontaneous venous pulsation is present in about 80% of patients, and it is not associated with headaches. B-scan of the optic discs is usually diagnostic, but a lack of calcification in children and adolescents can sometimes render this investigation unreliable. In such cases the optic discs have a pink appearance, and the edges are rarely completely obscured.
Idiopathic intracranial hypertension can cause papilledema with associated headaches. It usually affects young, overweight women. Patients frequently report worsening of the headaches with activities that increase intracranial pressure, such coughing or sneezing. They can have visual obscuration, tinnitus, and auditory sensations. CT scan may be normal, although there may be small or slitlike ventricles and an “empty sella sign.” Cerebrospinal fluid pressure is raised on lumbar puncture.
An intracranial space-occupying lesion will usually be detectable on head CT or will be associated with evidence of hydrocephalus. Hypertension is not a feature of these conditions.
This case is unusual because the intra-abdominal cyst seems to have caused hypertension and bilateral disc swelling in the absence of common funduscopic signs of hypertensive retinopathy. Whereas polycystic ovarian syndrome is known to cause hypertension through hemodynamic alterations and variations in peripheral vascular resistance, it is uncommon for bilateral disc swelling to be a presenting feature.(5,6) Moreover, the presence of a large solitary ovarian cyst does not fulfill the criteria of PCOS diagnosis.(7) We hypothesize that the size of the ovarian cyst may have had a role in compressing the renal veins, thus causing an associated hypertension and bilateral optic neuropathy.
Bilateral optic disc swelling secondary to malignant hypertension has been reported in children, although this is usually accompanied by, for example, retinal hemorrhages, exudates, or cotton wool spots.(8)
2. Lee AG, Beaver HA. Acute bilateral optic disk edema with a macular star figure in a 12-year-old girl. Surv Ophthalmol 2002;47:42-49.
3. Hayreh SS, Servais GE, Virdi PS. Fundus lesions in malignant hypertension. V. Hypertensive optic neuropathy. Ophthalmology 1986;93:74-87.
4. Kovach, Jaclyn L. Hypertensive optic neuropathy and choroidopathy in an 18-year-old woman with renal failure. Retinal Cases & Brief Reports 2010;4:187-9.
5. Alexander CJ, Tangchitnob EP, Lepor NE. Polycystic ovary syndrome: a major unrecognized cardiovascular risk factor in women. Rev Cardiovasc Med 2009;10:83-90.
6. Trakakis E, Balanika A, Kassanos D, et al. Hemodynamic alterations and wall properties in large arteries of young, normotensive, and non-obese women with polycystic ovary syndrome. J Endocrinol Invest 2008;31:1001-7.
7. Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group 2004 Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril 81:19–25.
8. Ba-Abbad RA, Nowilaty SR. Bilateral optic disc swelling as the presenting sign of pheochromocytoma in a child. Medscape J Med 200810:176.