A 7-week-old infant with right upper eyelid mass
Digital Journal of Ophthalmology 2010
Volume 16, Number 4
October 2, 2010
DOI: 10.5693/djo.03.2010.09.001
Volume 16, Number 4
October 2, 2010
DOI: 10.5693/djo.03.2010.09.001
Download PDF

Figure 1
Appearance of lesion at presentation.
Appearance of lesion at presentation.
Twelve days postoperatively, the patient was noted to have a recurrence, which continued to progress over the next two weeks. At that point (1 month postoperatively), the patient was given an intralesional corticosteroid injection (50/50 mix of 40 mg/mL triamcinolone and 6 mg/mL betamethasone). There was no recurrence at 2 months’ follow-up (Figure 4).
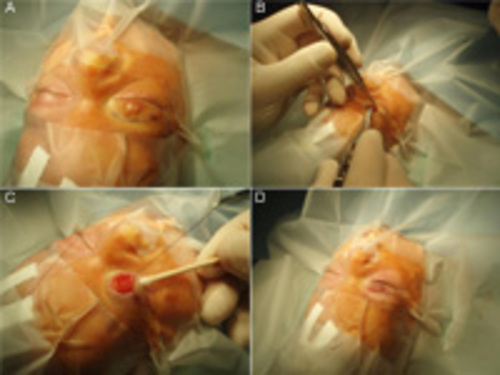
Figure 2
Surgical excision of right upper eyelid lesion. A, Preoperative patient preparation, with incision marked above eyelid crease. B, Incision made along previously noted mark. C, Exposure of eyelid mass. D, Postoperative photograph after mass excision and closure.
Surgical excision of right upper eyelid lesion. A, Preoperative patient preparation, with incision marked above eyelid crease. B, Incision made along previously noted mark. C, Exposure of eyelid mass. D, Postoperative photograph after mass excision and closure.
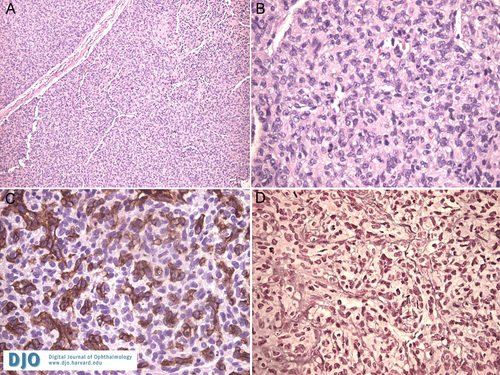
Figure 3
A, Histology demonstrating high cellularity with only rare vascular components (hematoxylin and eosin, original magnification ×40). B, On higher magnification, numerous mitotic figures were noted, reflecting a highly proliferative lesion (hematoxylin and eosin, ×200). C, A CD31 stain emphasizing the numerous endothelial channels in the lesion (×200). D, Positive reticulin stain surrounding capillary vessels (×200).
A, Histology demonstrating high cellularity with only rare vascular components (hematoxylin and eosin, original magnification ×40). B, On higher magnification, numerous mitotic figures were noted, reflecting a highly proliferative lesion (hematoxylin and eosin, ×200). C, A CD31 stain emphasizing the numerous endothelial channels in the lesion (×200). D, Positive reticulin stain surrounding capillary vessels (×200).

Figure 4
Patient 2 months postoperatively. Note the surgical scar visible on the right upper eyelid above the lid crease. There is no evidence of recurrence.
Patient 2 months postoperatively. Note the surgical scar visible on the right upper eyelid above the lid crease. There is no evidence of recurrence.
Numerous treatments exist for capillary hemangiomas. Small non-elevated lesions can frequently be observed. First-line treatment for larger lesions typically includes corticosteroids, which can be administered topically (0.05% clobetasol cream) for superficial lesions, by intralesional injection (40mg/mL triamcinolone and 6mg/mL betamethasone) for intermediate or periorbital lesions, and orally (2mg/kg/day) for refractory lesions.(7) Corticosteroids carry signifcant risk, with systemic corticosteroids potentially causing growth retardation, personality changes, infections, adrenal crisis, diabetes risk, and even rebound growth on cessation.(8) Topical clobetasol cream minimizes many of these risks but still causes dermal atrophy and pigmentary changes, and it can take several weeks to achieve a therapeutic response.(8) Intralesional corticosteroid injection is often used as a first-line treatment, although it adds the risk of central retinal artery occlusion, which has been reported in the contralateral eye as well.(8)
Pulsed-dye laser therapy has been shown to successfully treat flat superficial lesions or residual surface blood vessels after steroid treatment.(9) This therapy has been particularly useful in cosmetically significant areas, including the periocular region. Surgical excision may be employed in refractory cases, particularly with lesions that appear well circumscribed. These lesions are not typically encapsulated, so there is a potential for recurrence as well as a risk of bleeding and a risk associated with general anesthesia.(9)
Interferon alpha-2a, which has been shown to inhibit angiogenesis and endothelial cell migration and proliferation in vitro, has shown promise in refractory cases as well; however, its use has adverse effects, including motor developmental delay and spastic diplegia.(10)
Propranolol has shown great promise in the treatment of capillary hemangiomas.(11,12) In one study, 11 children with capillary hemangiomas were administered 2mg/kg/day of propranolol. Many of these patients began exhibiting color changes of their lesions within 24 hours, and all patients experienced resolution of their capillary hemangiomas, although varying treatment intervals were required.(11) It has been hypothesized that propranolol causes vasoconstriction of this highly vascular lesion and acts to down-regulate vascular endothelial growth factor and basic fibroblastic growth factor (bFGF), eventually triggering apoptosis of capillary endothelial cells.(11)
2. Schwartz SR, Kodsi SR, Blei F, Ceisler E, Steele M, Furlan L. Treatment of capillary hemangiomas causing refractive and occlusional amblyopia. J AAPOS;11(6):577-83.
3. Harris GJ, Sakol PJ, Bonavolonta G, De Conciliis C. An analysis of thirty cases of orbital lymphangioma: pathophysiologic considerations and management recommendations. Ophthalmology.1990; 97(12):1583-92.
4. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions. Ophthalmology 2004; 111:997-1008.
5. Li G, Lin T, Wu Q, Zhou Z, Gold MH. Clinical analysis of port wine stains treated by intense pulsed light. J Cosmet Laser Ther 2010; 2(1):2-6.
6. Miller NR, ed. Walsh and Hoyt’s Neuro-Ophthalmology. 4th ed. Baltimore: Williams & Wilkins; 1988;3:1296-1300.
7. Ranchod TM. Frieden IJ, Frederick DR. Corticosteroid treatment of periorbital haemangioma of infancy: a review of the evidence. Br J Ophthalmol 2005; 89(9):1134-8.
8. Boon LM, MacDonald DM, Mulliken JB. Complications of systemic corticosteroid therapy for problematic hemangioma. Plast Reconstr Surg 1999; 104(6):1616-23.
9. Azizkhan RG. Laser surgery: new applications for pediatric skin and airway lesions. Curr Opin Pediatr 2003;15(3):243-7.
10. Barlow CF, Priebe CJ, Mulliken JB, et al. Spastic diplegia as a complication of interferon alfa-2a treatment of hemangiomas of infancy. J Pediatrics 132(3):527-30.
11. Léauté-Labrèze C, Dumas de la Roque E, Hubiche T, Thambo JB,Taïeb A. Propranolol for severe hemangiomas of infancy. New England Journal of Medicine 2008;358(24):2649-51.
12. Cruz A, Siegfried EC. Propranolol treatment for periocular capillary hemangiomas. J AAPOS 2010;14(3):199-200.