A 37-year-old man with a black spot in his vision
Digital Journal of Ophthalmology 2010
Volume 16, Number 1
February 9, 2010
DOI: 10.5693/djo.03.2009.12.001
Volume 16, Number 1
February 9, 2010
DOI: 10.5693/djo.03.2009.12.001
Download PDF
The patient’s past medical history is significant for an episode of malaise and myalgias after his young daughter had gastroenteritis six months prior to his ocular complaints. His symptoms were followed by severe headaches and an acute episode of confusion and altered mental status. He was seen at an outside hospital and an MRI of the brain showed numerous white matter lesions, including lesions in the corpus callosum. He had mild pleocytosis of his cerebrospinal fluid (CSF). He was felt to have a postinfectious encephalopathy versus demyelinating disease and was treated with methylprednisolone. His cognitive symptoms improved significantly and there was some resolution of the white matter lesions on repeat MRI with no further treatment. He continued to complain of some mild residual fatigue which prevented him from working. Six months after his initial symptoms, he was re-admitted to the hospital for another episode of confusion and headache. There was no history of skin lesions. There were increased white matter lesions on MRI. Cerebrospinal fluid demonstrated elevated protein but a normal white blood cell count. An angiogram and a right frontal brain and leptomeningeal biopsy of one of the lesions were unrevealing. An extensive laboratory panel was negative. The patient’s symptoms improved with methylprednisolone, but he continued to have confusion and headaches on oral prednisone. The patient also began to complain of hearing loss.
The patient then began to have ocular complaints and ophthalmologic evaluation was performed serially.
The patient had a repeat examination 2 weeks later following worsening of neurologic symptoms. Examination at this time showed visual acuity of 20/20 in both eyes. The pupil exam was normal. There was significant superior visual field constriction in both eyes on confrontation. Dilated fundus exam showed large areas of retinal nonperfusion, multiple areas of arterial occlusion, and active vasculitis in both eyes (Figure 3). Fluorescein angiogram confirmed multiple areas of active vasculitis in both eyes (Figure 4).
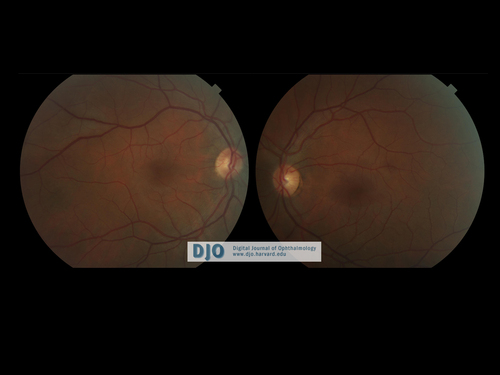
Figure 1
Fundus photos showing posterior pole OU on initial ophthalmologic exam.
Fundus photos showing posterior pole OU on initial ophthalmologic exam.

Figure 2
Fluorescein angiography demonstrating vascular occlusion OD and mild vasculitis OU.
Fluorescein angiography demonstrating vascular occlusion OD and mild vasculitis OU.
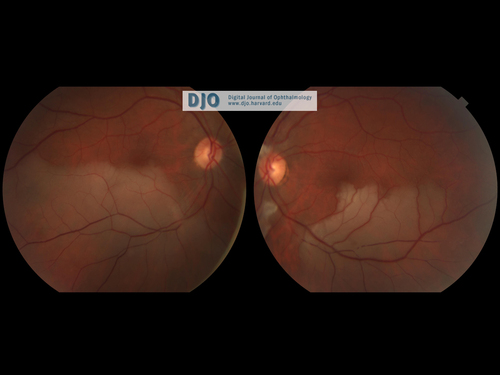
Figure 3
Fundus photos on repeat examination 2 weeks after initial exam showing significant areas of retinal vascular occlusions in both eyes with large areas of retinal nonperfusion OU and cotton wool spots OS.
Fundus photos on repeat examination 2 weeks after initial exam showing significant areas of retinal vascular occlusions in both eyes with large areas of retinal nonperfusion OU and cotton wool spots OS.
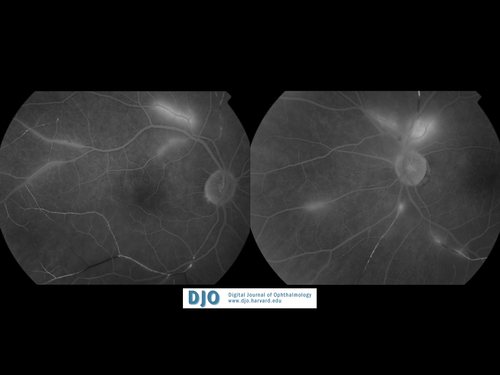
Figure 4
Fluorescein angiography demonstrating significant arteriolar occlusions OU and active retinal vasculitis OU.
Fluorescein angiography demonstrating significant arteriolar occlusions OU and active retinal vasculitis OU.
• ANA
• RF
• ds DNA
• anti-Ro
• anti-La
• C3/C4
• anti-RNP
• anti-Smith
• lupus anticoagulant
• Thyroid function tests
• Homocystine
• Lipoprotein a
• anticardiolipin antibody
• beta-2 glycoprotein
• ANCA
• Plasminogen activating inhibitor
• Protein C and S
• Factor V Leiden deficiency
• Antithrombin III
• Prothrombin gene mutation 20210
• Hemoglobin electropheresis
• Lyme antibody
• HBV
• HCV
• RPR
• Erlichia
• Babesiosis
• ACE
• HIV
• SPEP
• Cryocrit
• ESR
• C-reactive protein
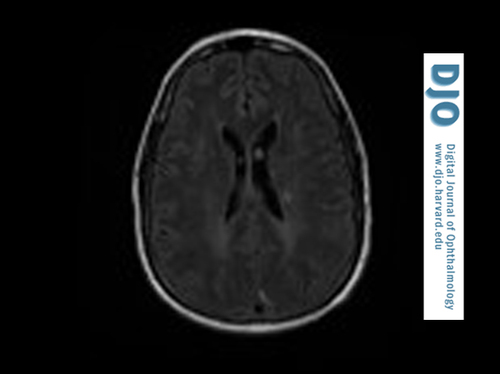
Figure 5
MRI (T2 FLAIR images): focal hyperintense lesions in the white matter and gray matter.
MRI (T2 FLAIR images): focal hyperintense lesions in the white matter and gray matter.
One week after this treatment was instituted, the patient’s visual acuity was stable, and the retinal vasculitis had markedly improved on fluorescein angiography.

Figure 6
Fluorescein angiography 1 week after initiating therapy with Solumedrol and cyclophosphamide with significant improvement in areas of vasculitis
Fluorescein angiography 1 week after initiating therapy with Solumedrol and cyclophosphamide with significant improvement in areas of vasculitis
• CNS vasculitis with retinal vasculitis: CNS vasculitis may present with headache and encephalopathy and may have associated retinal vasculitis. Protein levels in the CSF are elevated. Ischemic changes may be evident on neuroimaging and alterations in vessel caliber may be seen on cerebral angiography.
• Susac syndrome: This arteriolar microangiopathy affects pre-capillary arterioles in the brain, retina, and cochlea leading to encephalopathy, vision loss, and hearing loss.
• Multiple sclerosis: Focal neurologic signs and symptoms combined with white matter lesions on neuroimaging may be indicative of a demyelinating disease such as multiple sclerosis. Multiple sclerosis can also present with inflammation of the blood vessels in the retina with a perivasculitis.
• Systemic lupus erythematosus: SLE can involve multiple organ systems and cause vasculitis in the brain and retina. Inflammatory markers such as ANA are usually positive in this disease process; however, there are cases of SLE with negative antinuclear antibody tests. Other clinical signs of lupus, including skin rash, arthritis, and renal dysfunction are supporting signs for diagnosis of SLE.
• Behçet’s disease: Behçet’s disease can be associated with an occlusive vasculitis in the brain and retina. In addition to oral and genital ulcerations, ocular inflammation, and skin lesions, these patients may also have high frequency sensorineural hearing loss. The central nervous system may be affected in Behçet’s syndrome with development of confusional syndrome, meningoencephalitis, or brainstem involvement.
Susac syndrome is an arteriolar microangiopathy that affects the brain, retina, and cochlea, causing symptoms of encephalopathy, retinal vascular occlusions, and sensorineural hearing loss. It was originally described in 1979 by Susac, who reported on two cases of young women with this triad of symptoms.(1) Susac syndrome typically presents in younger patients, with ages ranging from 16-58. There is also a 3 to 1 predominance in women. The pathophysiology of Susac syndrome is still not well understood; however, it is believed to be an immune-mediated endotheliopathy affecting microvasculature of the brain, retinal vessels, and cochlea.(2) Brain biopsy of lesions in patients with Susac syndrome demonstrates microinfarcts in the cerebral cortex and white matter.(1) Muscle biopsies have also demonstrated endothelial cell necrosis and occlusion of small arterioles.(3)
As with this patient, the diagnosis of Susac syndrome may be difficult. The triad of symptoms may not manifest themselves concurrently, and visual and hearing deficits may be difficult to detect in encephalopathic patients. The differential diagnosis for Susac syndrome is extensive and includes demyelinating diseases such as multiple sclerosis and acute demyelinating encephalomyelitis (ADEM), CNS vasculitis, thromboembolic stroke, Behçet’s disease, and systemic lupus erythematosus. Ophthalmologic exam, including dilated fundoscopic examination and fluorescein angiography, can be helpful in identifying areas of retinal vascular occlusions and active retinal vasculitis.(4) FA may also be useful in tracking response to therapy, as in the improvement or resolution of vasculitis as seen in this case.(5) Neuroimaging may also be useful in the diagnosis as patients with Susac syndrome classically have lesions in the corpus callosum. Lesions are usually T2 hyperintense, may or may not enhance with contrast, and can be scattered in both the white matter and gray matter.(2) In some patients these hyperintense lesions may disappear as symptoms improve and return with exacerbation of disease. These findings may aid in the distinction between Susac syndrome and demyelinating diseases such as multiple sclerosis. The cerebrospinal fluid in patients with Susac syndrome may have elevated protein levels and mild pleocytosis.
The clinical course of Susac syndrome may be self-limited, with reports of symptom resolution from 6 months to 5 years following initiation of disease. Without treatment, the sequelae of Susac syndrome such as cognitive deficits, vision loss, and hearing loss can be quite severe.
The treatment of Susac syndrome is immunosuppression with high dose intravenous steroids and immunosuppressants such as cyclophosphamide, intravenous immunoglobulin, and rituximab.(3,4) There have also been reports of successful treatment with use of hyperbaric oxygen therapy.(6) Plasmapheresis has also been reported to result in improvement in cerebral deficits in some patients.(7) Anticoagulation has been proposed as a treatment option, but there have been no laboratory testing or histopathology to support a procoagulant state.(7) Patients who have been treated with anticoagulants or antiplatelet agents have continued to develop new symptoms during treatment. Of all the different treatment modalities, systemic steroids have been associated with improvement in symptoms and signs of Susac syndrome. While symptoms of active inflammation, including encephalopathy and retinal vasculitis, improve with immunosuppression, areas of prior infarction may result in permanent deficits in cognition, vision, or hearing. Delay in diagnosis can lead to permanent sequelae of the microangiopathic disease process. In some patients, symptoms may recur upon attempted taper of steroids and longer duration of immunosuppression may be needed to prevent exacerbations of disease.
2. Do TH, Fisch C, Evoy F. Susac syndrome: report of four cases and review of the literature. Am J Neuroradiol 2004;25(3):382-8.
3. Rennebohm RM, Susac JO. Treatment of Susac's syndrome. J Neurol Sci 2007;257(1-2):215-220.
4. Bitrian E, Sanchez-Dalmau B, Gilbert ME, Adan A, Susac JO. Retinal infarcts in a patient with an acute confusional syndrome. Surv Ophthalmol 2009;54(4):503-6.
5. Martinet N, Fardeau C, Adam R, et al. Fluorescein and indocyanine green angiographies in Susac syndrome. Retina 2007;27(9):1238-42.
6. Li HK, Dejean BJ, Tang RA. Reversal of visual loss with hyperbaric oxygen treatment in a patient with Susac syndrome. Ophthalmology 1996;103(12):2091-8.
7. Petty GW, Engel AG, Younge BR, et al. Retinocochleocerebral vasculopathy. Medicine (Baltimore) 1998;77(1):12-40.