A 68-year-old man with a recurrent orbital lesion
Digital Journal of Ophthalmology 2009
Volume 15, Number 4
September 2, 2009
Volume 15, Number 4
September 2, 2009
Download PDF

Figure 1a
External examination revealed a fixed mass that was painful on palpation as well as left hypoglobus.
External examination revealed a fixed mass that was painful on palpation as well as left hypoglobus.

Figure 1b
Photograph demonstrating proptosis of the left globe.
Photograph demonstrating proptosis of the left globe.
An orbital MRI was obtained. A polylobulated mass in the superolateral quadrant of the left orbit was found. There was apparent destruction of the lateral wall and lateral part of the orbital roof by the tumor. Upper eyelid infiltration was also seen. The globe itself was normal. (Figure 2a-b)
Pathology
An incisional biopsy was performed via an anterior orbitotomy. It revealed the presence of a malignant mixed tumor arising from a pleomorphic adenoma. Immunohistochemical studies with keratin 7 were also obtained and confirmed the presence of epithelial cells in the malignant clone. (Figure 3a-b)
A consultation with an oncologist was requested and an extensive systemic workup including cerebral MRI, PET scan, chest x-ray, abdominopelvic CT scan, CBC, renal and liver tests was ordered. All results were within normal limit. The remainder of the complete physical examination was normal.

Figure 2a
T1-weighted fat suppressed image showing the ill-defined mass in the left orbit. The lacrimal gland cannot be distinguished.
T1-weighted fat suppressed image showing the ill-defined mass in the left orbit. The lacrimal gland cannot be distinguished.

Figure 2b
T1-weighted fat suppressed image showing the tumor coming in close contact with the left lateral rectus muscle and its insertion on the globe. The optic nerve is intact. The lesion measures 5.1 x 3.4 x 2.4 cm.
T1-weighted fat suppressed image showing the tumor coming in close contact with the left lateral rectus muscle and its insertion on the globe. The optic nerve is intact. The lesion measures 5.1 x 3.4 x 2.4 cm.
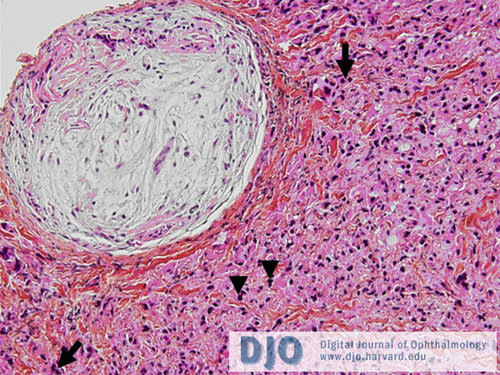
Figure 3a
Benign mixed tumor composed of clumps of ovoid and fusiform-shaped cells embedded in a myxoid stroma is seen in the upper left corner. The malignant component is on the right. Mitotic figures can be seen (arrows) as well as dense chromatin in the nuclei of cells showing an elevated nuclear-cytoplasmic ratio (arrowheads).
Benign mixed tumor composed of clumps of ovoid and fusiform-shaped cells embedded in a myxoid stroma is seen in the upper left corner. The malignant component is on the right. Mitotic figures can be seen (arrows) as well as dense chromatin in the nuclei of cells showing an elevated nuclear-cytoplasmic ratio (arrowheads).
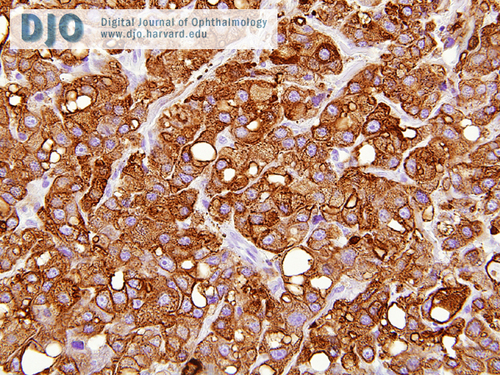
Figure 3b
Positive staining of the malignant cells for keratin 7, which confirms the epithelial origin of the tumor.
Positive staining of the malignant cells for keratin 7, which confirms the epithelial origin of the tumor.
One week later the patient developed necrosis of the distal portion of his temporoparietal flap and of the overlying skin graft. This exposed the Medpor™ implant. The patient was taken back to the operating room and the area was debrided and reconstructed with a radial forearm free flap. A left superficial parotidectomy with facial nerve dissection and a left cervical neck dissection were also performed since a tumor was found in the ipsilateral parotid gland on reviewing the MRI. All were free of malignancy. Surprisingly, an entirely benign pleomorphic adenoma was found in the ipsilateral parotid gland with no evidence of metastasis. The patient then received radiotherapy to the orbital region. Figure 6 shows him 3 months after the second procedure.

Figure 4
Perioperative image showing the extent of the defect.
Perioperative image showing the extent of the defect.
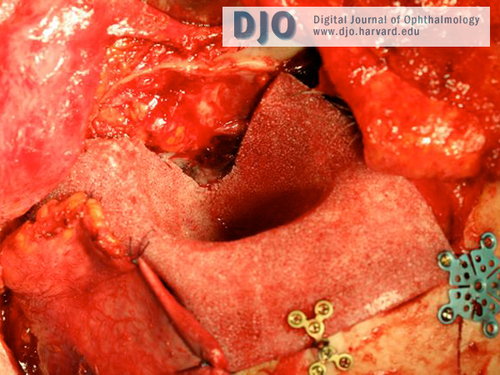
Figure 5
Orbit reconstructed with the MedporTM implant.
Orbit reconstructed with the MedporTM implant.

Figure 6
Picture taken 3 months after the last surgery.
Picture taken 3 months after the last surgery.
In our patient, the past history of an incompletely resected pleomorphic adenoma combined with the aggressiveness of the recurrence he was experiencing pointed to a diagnosis of carcinoma ex-pleomorphic adeoma (malignant mixed tumor).
Lacrimal gland lesions constitute almost 10% of all space-occupying orbital lesions. Between 50 and 80 percent are inflammatory or lymphoid tumors. Epithelial tumors, of which approximately 55 percent are benign and 45 percent malignant, represent the vast majority of remaining lesions.(1,2)
Pleomorphic adenoma is the most common benign neoplasm of the lacrimal gland, and it is almost always found in the orbital lobe of the gland. It tends to affect men slightly more than women. Typically, a patient between 40 and 50 years of age will present with a slowly progressive and painless proptosis. Globe dystopia is commonly seen. Orbital imaging shows a well-circumscribed mass usually without bony erosion. Histopathologically, these lesions consist of a mixture of epithelial, myoepithelial and mesenchymal elements that led to the term benign mixed tumor. Management consists of complete surgical excision of the tumor with its pseudocapsule and a surrounding margin of orbital tissue. Incisional biopsy prior to surgery should be avoided. One series found a recurrence rate of 32 percent at 5 years in previously biopsied lesions, compared to 3 percent for those without biopsy.(3) This surgical dictum has however come under recent debate.(4)
Of recurrent pleomorphic adenomas, it is estimated that 10 percent will become malignant after 20 years and that 20 percent will become malignant after 30 years.(3) Malignant transformation will result in a malignant mixed tumor, termed carcinoma ex-pleomorphic adenoma. Patients are typically older than those with pleomorphic adenoma, and they present with a rapidly growing painful lesion. Bony erosion is commonly seen on orbital imaging. Histopathologic diagnosis can only be made if one has either earlier biopsy evidence of a pre-existent pleomorphic adenoma, or if the coexistence of vestiges of a pleomorphic adenoma is seen along with the outgrowth of a malignant clone in the material.(5) Most commonly, the malignant epithelial elements will be a poorly differentiated adenocarcinoma, but adenoid cystic carcinomas have also been described.(6) Incisional biopsy is recommended to confirm the diagnosis and a systemic workup for metastasis should be conducted. Malignant mixed tumors that have invaded beyond their capsule carry a poor prognosis, with a survival rate at 5 years of only 35 to 45 percent.(7) Management consists of some form of radical exenteration followed by adjunctive radiotherapy. As regional metastases have been described months after orbital surgery, it might be advisable to perform parotid and cervical lymph node dissections at the time of the first intervention.(5)
This case illustrates the potentially devastating hazards of an incompletely resected pleomorphic adenoma. It is important that such tumors be completely excised during the initial surgery to prevent recurrences and possible malignant transformation.
2. Font RL, Smith SL, Bryan RG. Malignant epithelial tumors of the lacrimal gland: a clinicopathologic study of 21 cases. Archives of Ophthalmology 1998;116:613-616.
3. Font RL, Gamel JW. Epithelial tumors of the lacrimal gland: an analysis of 265 cases. In: Jakobiec FA, ed. Ocular and Adnexal Tumors. New York: Aesculapius, 1978;787–805.
4. Lai T, Prabhakaran VC, Malhotra R, Selva D. Pleomorphic adenoma of the lacrimal gland: is there a role for biopsy? Eye 2009;23(1):2-6.
5. Jakobiec FA, Font RL. Orbit. In: Spencer WH, ed. Ophthalmic Pathology. Philadelphia: WB Saunders Company, 1986; chap. 12.
6. Ni C, Kuo PK, Dryja TP. Histopathological classification of 272 primary epithelial tumors of the lacrimal gland. Chinese Medical Journal 1992;105:481-485.
7. Rootman J. Diseases of the orbit: a multidisciplinary approach. Philadelphia: Lippincott Williams & Wilkins, 2003; 351-60.