A 29-year-old man with a 3-month history of blurred vision and micropsia in the left eye
Digital Journal of Ophthalmology 2008
Volume 14, Number 17
September 5, 2008
Volume 14, Number 17
September 5, 2008
Ocular coherence tomography (OCT) of the left eye revealed schisis-like separation of the retinal layers in the macula with a partial outer layer detachment adjacent to the disc and strands of tissue bridging the schisis cavity (Figure 2). A connection between the inner layer separation and the optic disc was suggested. Mean central 1 mm retinal thickness was 697 microns. Visual acuity deteriorated 2 months after presentation to 6/18 (20/60).
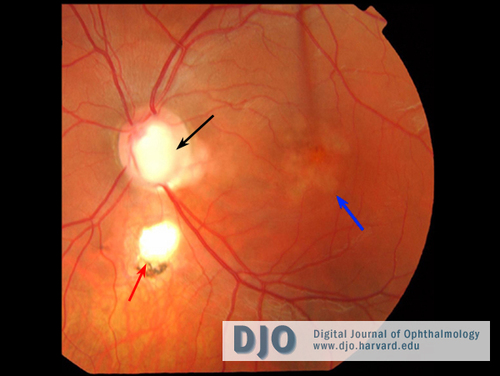
Figure 1
Color fundus photograph of the left eye showing the colobomatous disc (black arrow), retino-choroidal coloboma (red arrow), foveal retinal pigment epithelial atrophy and macular elevation (blue arrow).
Color fundus photograph of the left eye showing the colobomatous disc (black arrow), retino-choroidal coloboma (red arrow), foveal retinal pigment epithelial atrophy and macular elevation (blue arrow).
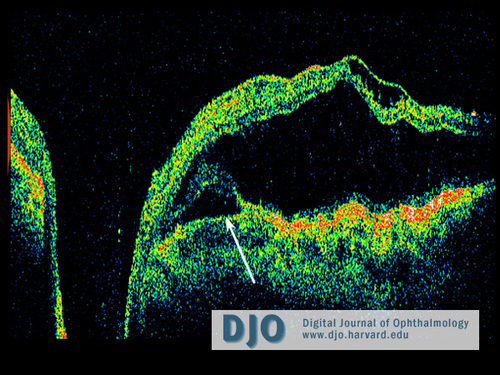
Figure 2
Linear horizontal OCT image pre-treatment through the disc. The scan shows schisis-like separation of the retinal layers in the macula with a partial outer layer detachment adjacent to the disc (arrow).
Linear horizontal OCT image pre-treatment through the disc. The scan shows schisis-like separation of the retinal layers in the macula with a partial outer layer detachment adjacent to the disc (arrow).
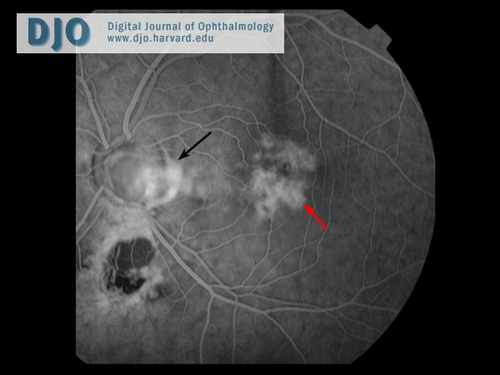
Figure 3
Fluorescein angiogram 33 seconds. There is leakage within the coloboma and between the disc and the fovea (black arrow). Patchy retinal pigment epithelial atrophy can be seen around the fovea (red arrow).
Fluorescein angiogram 33 seconds. There is leakage within the coloboma and between the disc and the fovea (black arrow). Patchy retinal pigment epithelial atrophy can be seen around the fovea (red arrow).
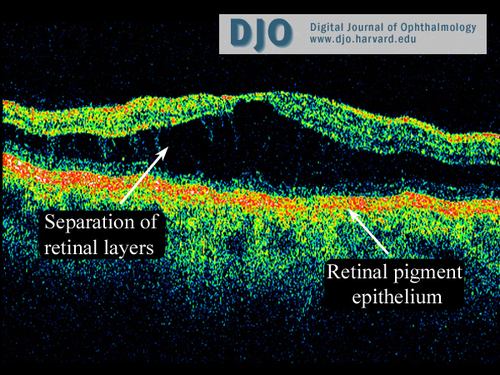
Figure 4
Linear horizontal OCT scan through the macula 6 months after treatment.
Linear horizontal OCT scan through the macula 6 months after treatment.
In CSR there is a localized serous detachment of the neurosensory retina in the region of the macula secondary to focal RPE defects. There is no optic disc pit seen as in this case. In CSR, fluorescein angiography can show a ‘smoke-stack’ appearance, which was not seen in this case either. The lack of these findings excludes this as the diagnosis.
Retinal pigment epithelial detachment (PED)
PED is probably caused by reduction of the hydraulic conductivity of the thickened Bruch’s membrane, thus impeding movement of fluid from the RPE towards the choroid. OCT images show separation of the RPE from Bruch’s membrane by the fluid in PED. There is no sub-RPE fluid in this case, and the clinical appearance excludes this as the diagnosis.
Age related macular degeneration (AMD)
AMD usually affects patients over the age of 50 years and is the most common cause of irreversible visual loss in the developed world. Clinical features include the presence of drusen, pigment epithelial alterations, hemorrhages, choroidal neovascularization and RPE detachment. In view of the age of this patient (29 years) and the lack of other AMD clinical features, this is not the diagnosis.
Lincoff and Kreissig have described the treatment of optic disc pits associated with macular retinoschisis with pneumatic displacement.(1) Lincoff et al.(2) were the first to describe schisis-like separation of the inner retinal layers combined with outer layer detachment associated with optic disc pits using stereo photography. With the advent of OCT, the complex bi-laminar retinal separation has been further elucidated,(3) and a connection between the inner layer separation and the disc pit has been identified.(1) Bridging strands of tissue could contain Henle’s fibers which would explain why, unlike true retinoschisis, there is not an absolute scotoma. Outer layer detachment can be progressive and may be the critical feature causing a drop in visual acuity.(1) Although serous macular detachment is the most common sequela leading to vision loss in these patients, the origin of the fluid remains to be elucidated. Theories have implicated fluid entry from either the vitreous cavity or cerebrospinal fluid via the peripapillary subarachnoid space.(4, 5) In addition, outer layer holes can develop resulting in visual loss.(2) However, resolution of maculopathy spontaneously (2, 6) or with bed rest and eye padding (6) has also been described, and visual acuity can then improve.
Approaches to the treatment of optic disc pit maculopathy have included laser adjacent to the optic disc,(6) pneumatic displacement,(1, 2) and vitrectomy with gas tamponade.(6, 7) In this case, the patient had confluent laser treatment to form adhesions and prevent accumulation of fluid under the retina. The laser uptake is within the retinal pigment epithelial layer; hence, this should not affect the retinal nerve fiber layer.
Lincoff and Kreissig (1) described the use of pneumatic displacement without laser in 3 patients with optic disc pit maculopathy using 0.4 to 0.6 ml of 100% C2F6. After 3 weeks of posturing, OCT was used to assess the results. Displacement was achieved in two patients (one of whom also had a macular hole in the outer layer) with reattachment of the outer layer detachment, reduction in inner layer separation and improvement in visual acuity to 20/40 in both. Interestingly, like our patient, the inner layer separation did not resolve, but nonetheless vision did improve. They stated that visual acuity had improved in 9 of 12 patients treated in this way. Unfortunately, the effect can be temporary with visual deterioration coinciding with the reappearance of outer layer detachment.
Schatz and McDonald (6) and Bakri and Beer (7) described vitrectomy with air or gas tamponade preceded by peripapillary laser in 3 and 2 patients, respectively. Schatz and McDonald (6) reported improved visual acuity in all cases with a minimum of 22 months follow up and a range of final visual acuities of 20/40 to 20/100. Bakri and Beer’s (7) patients maintained improved visual acuity for the 6 months of follow up. Hirakata et al.(8) achieved reattachment of 10 of eleven eyes with maculopathy associated with optic disc pits using pars plana vitrectomy without laser. They considered that induction of posterior vitreous detachment (PVD) was important for long-term success. Retinal damage caused by induction of PVD in one 15-year-old patient resulted in a poor visual outcome, but otherwise visual outcomes were good. In view of the reported difficulty in inducing a PVD and potential retinal complications, the initial management choice in this case was to perform pneumatic displacement without a vitrectomy. Recurrence rates are high in such cases and may then require a vitrectomy.
Our case lends support to the use of pneumatic displacement for maculopathy associated with optic disc colobomas with an improvement in visual acuity, resolution of outer layer detachment and reduction in inner layer separation maintained at 6 months. Vitrectomy with induction of a posterior vitreous detachment has also been demonstrated to be effective.(8)
2. Lincoff H, Lopez R, Kreissig I, Yannuzzi L, Cox M, Burton T. Retinoschisis associated with optic nerve pits. Arch Ophthalmol 1988;106:61-7.
3. Rutledge BK, Puliafito CA, Duker JS, Hee MR, Cox MS. Optical coherence tomography of macular lesions associated with optic nerve head pits. Ophthalmology 1996;103:1047-53.
4. Sugar HS. Congenital pits in the optic disc with acquired macular pathology. Am J Ophthalmol 1962;53:307–311.
5. Gass JDM. Serous detachment of the macula secondary to congenital pit of the optic nerve head. Am J Ophthalmol 1969;67:821–841.
6. Schatz H, McDonald R. Treatment of sensory retinal detachment associated with optic nerve pit or coloboma. Ophthalmology 1988;95:178-86.
7. Bakri SJ, Beer PM Vitreoretinal surgery for optic pit associated serous macular detachment. Int Ophthalmol 2004;25:143-6.
8. Hirakata A, Okada AA, Hida T. Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology 2005;112:1430-5.