A 25-month-old girl with vision loss, nystagmus, and anomalous head posture
Digital Journal of Ophthalmology 2009
Volume 15, Number 1
February 23, 2009
Volume 15, Number 1
February 23, 2009
Download PDF
Additional examination revealed full versions and ductions and a comitant esotropia. The patient had a left AHP, preferring right gaze. She had variable, symmetric, conjugate, small-to-moderate amplitude, and moderate-to-high frequency multiplanar involuntary ocular oscillations with a null position in right gaze of 30-40 degrees. There was no latent component and saccades, pursuit, and vestibulo-ocular reflexes were otherwise normal.

Figure 1
Fundus photograph of left optic nerve showing extreme cupping and atrophy present in both nerves at the time of diagnosis.
Fundus photograph of left optic nerve showing extreme cupping and atrophy present in both nerves at the time of diagnosis.
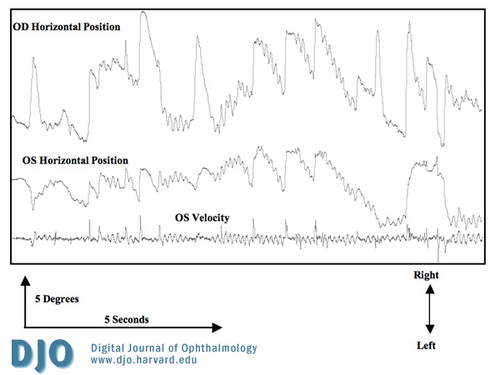
Figure 2
Ocular motility recording showing position trace OU and velocity trace OS at the time of diagnosis (right gaze is up and left gaze is down). The recording shows well-developed jerk and bidirectional jerk waveforms with periods of foveation, typical of infantile nystagmus syndrome.
Ocular motility recording showing position trace OU and velocity trace OS at the time of diagnosis (right gaze is up and left gaze is down). The recording shows well-developed jerk and bidirectional jerk waveforms with periods of foveation, typical of infantile nystagmus syndrome.
In this case, detailed examination of the patient revealed elevated intraocular pressures, severe myopia, Haab’s striae, and enlarged optic cups with pallor and deep cupping. The combination of these findings point to advanced infantile glaucoma.
The reduction in the patient’s IOP to an acceptable range had profound effects on her vision and ocular anatomy. Her myopia was significantly reduced and the optic discs demonstrated reversal of cupping. This latter finding is common in congenital glaucoma and differentiates it from the adult glaucomas. As her vision improved the nystagmus and AHP decreased. The development of INS in this patient is a result of poor ocular motor calibration due to associated glaucomatous sensory system deficits (optic neuropathy, myopia, corneal irregularities and strabismus).
INS is the most predominant type of ocular oscillation associated with visual deprivation.(2,4,8) Although the exact etiology of INS is unknown, it likely caused by abnormal communication between the developing sensory and motor systems leading to a defect of ocular motor calibration. Patients with INS typically present with a horizontal nystagmus characterized by a slow and fast phase that increases in intensity with fixation and decreases with sleep, inattention or convergence. The oscillations change direction about a neutral position and a null point in eccentric gaze manifests as an AHP.(9) Diagnosis is confirmed by oculography that demonstrates waveforms having slow phases that display an increasing velocity exponential curve associated with periods of foveation. AHP is strongly associated with INS.(9) Treatment of AHP due to an eccentric gaze null zone associated with INS is directed towards returning the head to a more normal position and decreasing the intensity of the oscillation. In this case, treatment of the glaucoma, myopia and strabismus improved vision and resulted in a decrease in the nystagmus and the AHP. Recognition of congenital glaucoma in this patient who presented with new-onset nystagmus and AHP was essential in preventing eventual blindness.
2. Robb RM, Petersen RA. Outcome of treatment for bilateral congenital cataracts. Ophthalmic Surg 1992;23:650-6.
3. Tusa RJ, Repka MX, Smith CB, Herdman SJ. Early visual deprivation results in persistent strabismus and nystagmus in monkeys. Invest Ophthalmol Vis Sci 1991; 32(1): 134-41.
4. Hertle RW, Dell'Osso LF. Clinical and ocular motor analysis of congenital nystagmus in infancy. J AAPOS 1999;3(2):70-9.
5. Mandal AK, Naduvilath TJ, Jayagandan A. Surgical results of combined trabeculotomy-trabeculectomy for developmental glaucoma. Ophthalmology 1998;105(6):974-82.
6. Gramer E, Tausch M, Kraemer C. Time of diagnosis, reoperations and long-term results of goniotomy in the treatment of primary congenital glaucoma: a clinical study. Int Ophthalmol 1996;20(1-3):117-23.
7. Tsamparlakis J, Alexakis J, Stavropoulos A. Visual development in successfully treated cases of congenital glaucoma. Child Care Health Dev 1979;5(6):431-8.
8. Spierer A. Etiology of reduced visual acuity in congenital nystagmus. Ann Ophthalmol 1991; 23(10):393-7.
9. Hertle RW, Zhu X. Oculographic and clinical characterization of thirty-seven children with anomalous head postures, nystagmus, and strabismus: the basis of a clinical algorithm. J AAPOS 2000; 4(1): 25-32.