A 34-year-old man with visual complaints and a tapetal-like reflex
Digital Journal of Ophthalmology 2008
Volume 14, Number 14
July 28, 2008
Volume 14, Number 14
July 28, 2008
He had poor vision in the right eye since childhood, which he attributed to trauma. His brother also had a history of poor vision. The patient had no other significant medical history.
Dilated fundus examination showed pallor and significant cupping of the optic disc in the right eye. There was a striking yellow-gold sheen to the posterior retina (Figure 1). In the left eye, the disc was normal. There was a similar, but more marked, yellow-gold sheen that extended anterior to the vascular arcades (Figure 3). The sheen was less marked in both eyes after 1 hour of dark adaptation (Figures 2 and 4).

Figure 1
Fundus photo of the right eye. The dilated examination showed pallor and significant cupping of the optic disc. While there were no definite abnormalities observed in the macula, a striking yellow-gold sheen to the retina was observed, particularly posteriorly.
Fundus photo of the right eye. The dilated examination showed pallor and significant cupping of the optic disc. While there were no definite abnormalities observed in the macula, a striking yellow-gold sheen to the retina was observed, particularly posteriorly.
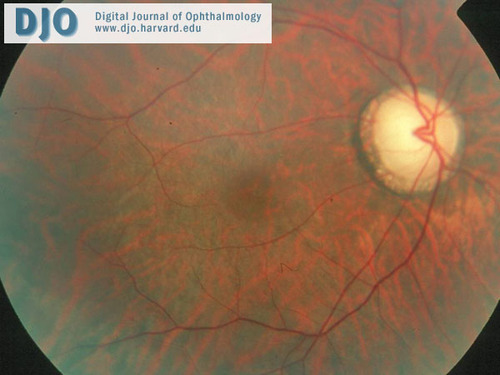
Figure 2
The tapetal-like sheen in the right eye was less marked after one hour of dark adaptation.
The tapetal-like sheen in the right eye was less marked after one hour of dark adaptation.

Figure 3
Fundus photo of the left eye. A normal disc and unremarkable macula are noted, but there is a marked golden-yellow sheen to the fundus extending beyond the arcades.
Fundus photo of the left eye. A normal disc and unremarkable macula are noted, but there is a marked golden-yellow sheen to the fundus extending beyond the arcades.
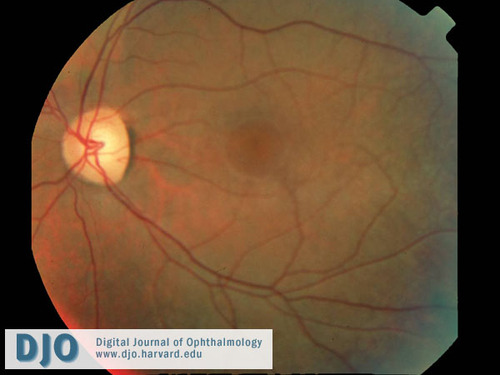
Figure 4
The tapetal-like sheen of the left fundus was less marked after one hour of dark adaptation.
The tapetal-like sheen of the left fundus was less marked after one hour of dark adaptation.
A full-field ERG was performed according to the international standard protocol. Results were compared to a database of healthy individuals or patients with no abnormal ERG values obtained in our lab. The patient’s ERG showed a reduced dim scotopic response in the right eye and a normal result in the left eye (Figure 5). The bright scotopic b-wave amplitude was reduced in both eyes but implicit times were normal (Figure 6). The bright photopic single flash response was non-recordable in both eyes (Figure 7). The 30Hz flicker responses were severely reduced in both eyes (Figure 8). The implicit time was borderline in the right eye and normal in the left eye.
Humphrey Visual Field (HVF) testing:
The left visual field showed severe constriction. The test could not be performed in the right eye.
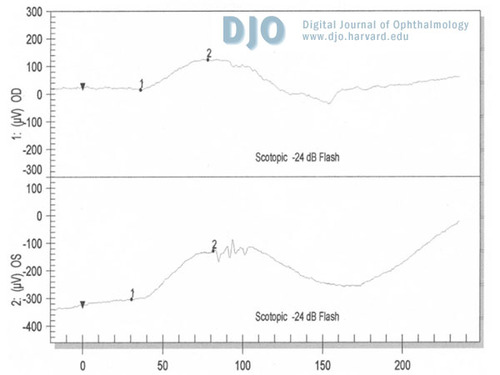
Figure 5
A mildly reduced dim scotopic response was seen in the right eye and a normal result in the left eye.
A mildly reduced dim scotopic response was seen in the right eye and a normal result in the left eye.
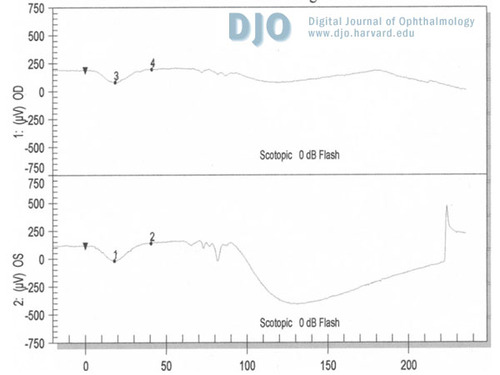
Figure 6
The bright scotopic b-wave amplitude was reduced in both eyes. However, implicit times were normal.
The bright scotopic b-wave amplitude was reduced in both eyes. However, implicit times were normal.
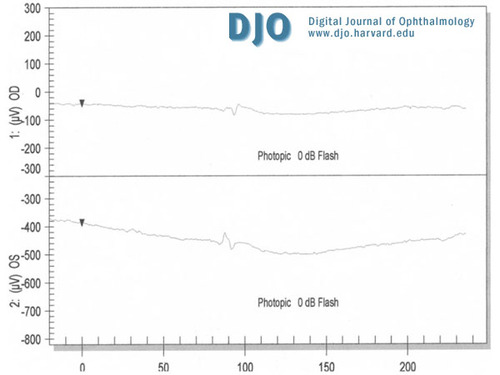
Figure 7
The bright photopic single flash response was non-recordable in both eyes.
The bright photopic single flash response was non-recordable in both eyes.
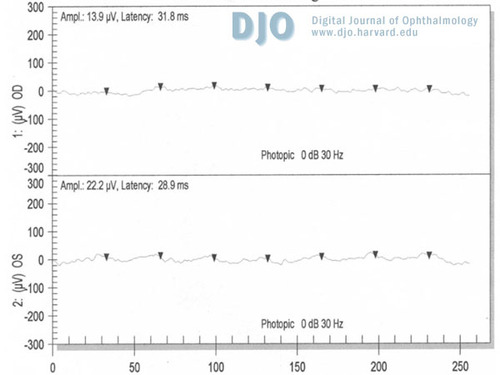
Figure 8
The 30 Hz flicker responses were severely reduced in both eyes.
The 30 Hz flicker responses were severely reduced in both eyes.
The origin of this phenomenon is unknown. Excessive extracellular potassium in the retina has been hypothesized, but not proven as the pathophysiological basis of the Mizuo-Nakamura phenomenon.(5) A case report of retinal detachment seen in a patient with Oguchi disease reported that the detached retina lost its golden reflex, but partially regained the reflex 7 months after segmental buckling surgery. The area of the golden sheen had enlarged during the following 14 months. This result suggested that a connection between the retinal pigment epithelium and sensory retina must be necessary for the abnormal fundus reflex to occur.(8) In another patient with Oguchi disease, diffuse, fine, white particles, which do not exist in normal subjects, were clearly demonstrated in the light-adapted retina with helium-neon laser. These particles were not seen by scanning laser ophthalmoscopy with the use of argon and infrared lasers, suggesting that they appear to be located in the outer retina, retina pigment epithelium, or both.(9) The time course of disappearance and appearance of the white particles correlated with the change in fundus color, suggesting that these particles contribute to the abnormal fundus coloration and Mizuo-Nakamura phenomenon. The authors proposed that these particles may be products of an abnormal metabolic pathway that operates during light adaptation.
In the present case, after excluding other possible causes of loss of consciousness, the episode of syncope was considered most likely related to a situational syncope due to a neurally-mediated reflex that occurs during urination or immediately thereafter.(10)
The poor vision in the right eye was probably related to the history of trauma during childhood, which could explain the traumatic optic neuropathy seen in the right eye during the fundus examination. The hypertelorism and shallow orbits findings were unrelated to the diagnosis. In addition, the ERG was performed by standardized methods designed to test separately the cone system with the photopic and flicker responses and the rod system with the scotopic responses. According to our findings, the ERG suggests a cone dystrophy. A cone-rod degeneration is a less likely possibility. In Oguchi's disease, the classic ERG findings show non-recordable scotopic responses after 30 minutes of dark adaptation and normal photopic and 30Hz flicker responses.(11)
The Mizuo-Nakamura phenomenon has been reported in X-linked cone dystrophy.(1) It has not been reported in cone-rod degeneration. This suggests that cone dystrophy is the likely diagnosis.
The typical visual symptoms and exam findings in cone dystrophy are photophobia, loss of visual acuity, loss of color, and central vision abnormalities. There is exclusive cone system involvement found on the ERG. Nevertheless, in some progressive forms, the rod system may be affected. The fundus examination is characterized by central macular pigment epithelial atrophy, although early cases may appear normal. In some cases, only a faint granular appearance may be present in the macula, while in others a bull’s eye pattern of the macula is evident. Visual acuity often declines to 20/200 by the end of the third decade.(12)
2. Pinckers A, Deutman AF. X-linked cone dystrophy. An overlooked diagnosis? International Ophthalmology. 1987; 10: 241-3.
3. Noble KG, Margolis S, Carr R. The golden tapetal sheen reflex in retinal disease. Am J Ophthalmol. 1989; 107: 211-17.
4. Oguchi C. Ueber einen Fall von eigenartiger Hemeralopie. Nippon Ganka Gakkai Zasshi. 1907; 11: 123.
5. de Jong PT, Zrenner E, van Meel GJ, Keunen JE, van Norren D. Mizuo Phenomenon in X-linked Retinoschisis. Pathogenesis of the Mizuo phenomenon. Arch Ophthalmol. 1991; 109: 1104-8.
6. Mizuo G. A new discovery in dark adaptation in Oguchi’s disease. Acta Soc Ophthalmol Jpn. 1913; 17: 1148.
7. Nakamura B. A new phenomenon of color change in the human fundus oculi in connection with the examination of adaptation to darkness. Klin Monatsbl Augenheilkd. 1920; 65: 83.
8. Abe T, Sato N, Sakuragi S. A case of Oguchi disease with rhegmatogenous retinal detachment. In Abstracts of the 53rd Annual Meeting of Japanese Clinical Ophthalmological Symposium. 1999; p 417.
9. Usui T, Ichibe M, Ueki S, Takagi M, Hasegawa S, Abe H, Sekiya K, Nakazawa M. Mizuo phenomenon observed by scanning laser ophthalmoscopy in a patient with Oguchi disease. Am J Ophthalmol. 2000; 130: 359-61.
10. Brignole M. Neurally-mediated syncope. Ital Heart J. 2005; 6: 249-55.
11. Dryja TP. Molecular genetics of Oguchi disease, fundus albipunctatus, and other forms of stationary night blindness: LVII Edward Jackson Memorial Lecture. Am J Ophthalmol. 2000; 130: 547-63.
12. Reichel E, Bruce AM, Sandberg MA, Berson EL. An electroretinographic and molecular genetic study of X-linked cone degeneration. Am J Ophthalmol. 1989; 108: 540-7.