A 23-year-old man with a cystic iris lesion
Digital Journal of Ophthalmology 2008
Volume 14, Number 15
August 1, 2008
Volume 14, Number 15
August 1, 2008
The patient was treated with cycloplegia and asked to return in 1 month, at which time the visual acuity had fallen to 20/70. IOP was still in the mid-teens. The cyst had enlarged to 8.0 mm x 4.5 mm and was encroaching on the visual axis (Figure 2). The decline in vision was attributed to this encroachment on the visual axis, as there was no evidence of any other anterior segment or fundus abnormalities. Cycloplegia was continued to provide the patient with a larger pupil. He was asked to return in 1 month for ultrasound biomicroscopy and re-examination.
At the next visit, visual acuity was stable at 20/70, and IOP was 17 mm Hg. The cyst now measured 10.0 mm x 8.0 mm and appeared to be obscuring the visual axis (Figure 3).

Figure 1
Initial appearance of cyst (three months after ruptured globe).
Initial appearance of cyst (three months after ruptured globe).

figure 2
Cyst progression over one month (4 months after open globe).
Cyst progression over one month (4 months after open globe).
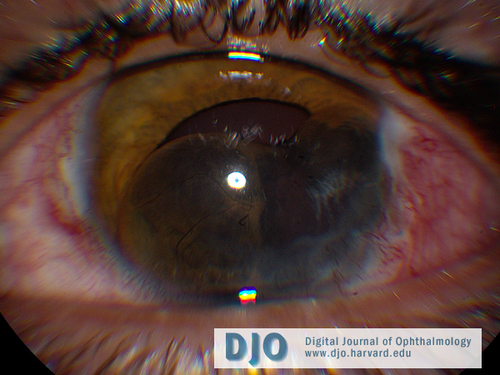
Figure 3
Cyst progression over two months (five months after ruptured globe).
Cyst progression over two months (five months after ruptured globe).
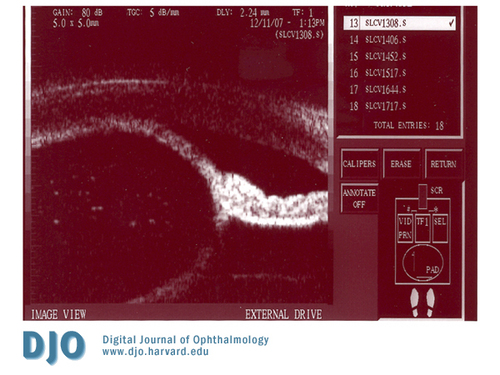
Figure 4
UBM showing cyst walls made up of anterior and posterior iris.
UBM showing cyst walls made up of anterior and posterior iris.
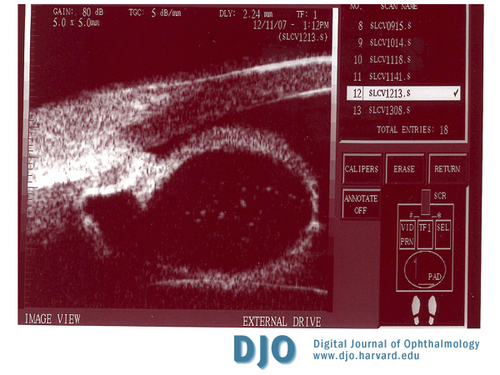
Figure 5
UBM centered near ciliary body.
UBM centered near ciliary body.
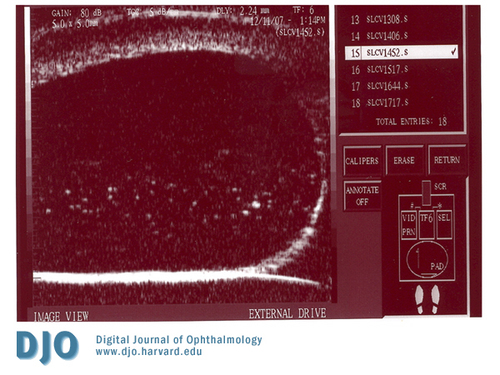
Figure 6
UBM showing anterior-posterior extent of cyst.
UBM showing anterior-posterior extent of cyst.
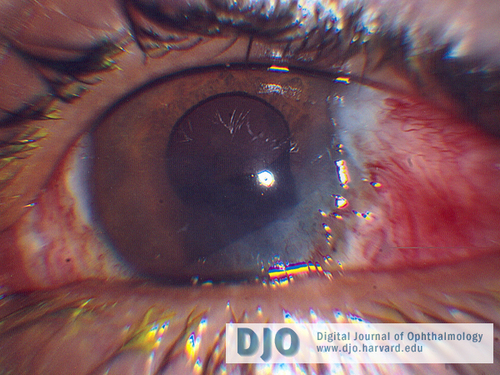
Figure 7
Cyst collapsed on Post-operative day 1.
Cyst collapsed on Post-operative day 1.

Figure 8
Cyst collapsed on post-operative week 2.
Cyst collapsed on post-operative week 2.
Upon review of the literature, we decided to use the alcohol injection described by Behrouzi and Khodadoust.(2) Other possible treatment regimens have been described including cryotherapy, photocoaugulation, en-bloc excision, and Mitomycin C injection.(3-7) These are all viable options, and there are advantages and disadvantages to each. Given our patient's relatively good vision and lack of any painful symptoms, we decided to use a minimalistic approach initially. At the last follow-up the patient continued to do well; the cyst remained collapsed, and there was only minimal post-operative intraocular inflammation. If there is recurrence of the cyst, a different approach may be considered. The patient's visual acuity did show a line of improvement immediately after draining the cyst. However, the patient has now developed a posterior subcapsular cataract that is the most likely cause of his decreased vision, since the cornea remains clear, and the fundus appears normal without any clinical evidence of macular edema. Cataract extraction will be considered in the future after the patient has fully recovered from this cyst evacuation procedure.
2. Behrouzi Z, Khodadoust A. Epithelial iris cyst treatment with intracyst ethanol irrigation. Ophthalmology 2003; 110:1601-1605.
3. Maumenee AE, Paton D, Morse PH, et al. Review of 40 histologically proven cases of epithelial downgrowth following cataract extraction and suggested surgical management. Am J Ophthalmol 1970; 69:598–603.
4. Naumann GOH, Rummelt V. Block excision of cystic and diffuse epithelial ingrowth of the anterior chamber: report on 32 consecutive patients. Arch Ophthalmol 1992; 110:223–7.
5. Sihota R, Tiwari HK, Azad RV, et al. Photocoagulation of large iris cysts. Ann Ophthalmol 1988; 20:470–2.
6. Sugar J, Jampol LM, Goldberg MF. Argon laser destruction of anterior chamber implantation cysts. Ophthalmology 1984; 91:1040–4.
7. Yu CS, Chiu SI, Tse RKK. Treatment of cystic epithelial downgrowth with intralesional administration of Mitomycin C. Cornea 2005; 24(7):884-886.