A 24-year-old woman with blurred vision and eye pain
Digital Journal of Ophthalmology 2008
Volume 14, Number 16
August 18, 2008
Volume 14, Number 16
August 18, 2008
The neurological examination was normal. Visual field testing showed a diffuse reduction in sensitivity of the left eye with a dense centrocecal scotoma and a superior temporal quadrantanopia in the right eye (Figure 1), which was confirmed with a second visual field test on the following day (Figure 2). This pattern of defects is a junctional scotoma.
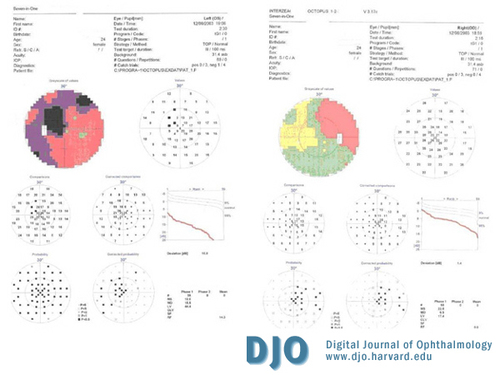
Figure 1
Dense cecocentral scotoma with diffuse reduction of the sensitivity of the left eye associated with a superior temporal quandrantanopia in the right eye (junctional scotoma).
Dense cecocentral scotoma with diffuse reduction of the sensitivity of the left eye associated with a superior temporal quandrantanopia in the right eye (junctional scotoma).
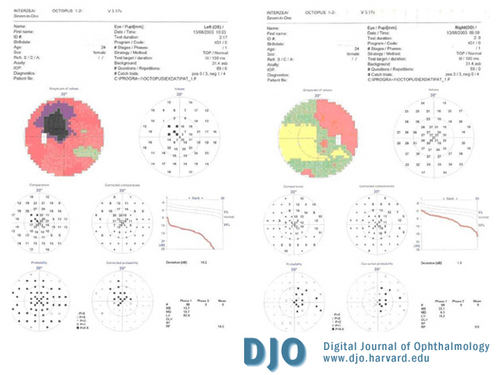
Figure 2
Similar junctional scotoma confirmed on the following day.
Similar junctional scotoma confirmed on the following day.
Blood work revealed a normal B12 level, negative antinuclear antibody (ANA) level, negative anti-double stranded DNA antibody level, and normal angiotensin converting enzyme level. Chest x-ray showed no evidence of interstial lung disease or hilar adenopathy.
The patient also underwent magnetic resonance imaging (MRI) of the brain and orbits, which revealed lesions consistent with demyelinating disease at the junction of the left optic nerve and optic chiasm. This is shown on T1-weighted, gadolinium-enhanced scans (Figure 3a). On T1-weighted scans, there were also multiple periventricular demyelinating lesions consistent with demyelinating disease (Figure 3b).
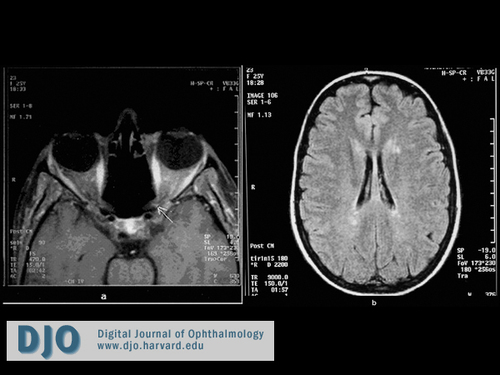
Figure 3
T1-weighted, gadolinium-enhanced MRI of brain and orbits. (a) Lesions consistent with demeylination plaques on the left side of the optic chiasm (arrow). (b) Lesions consistent with demyelinating areas in the periventricular region.
T1-weighted, gadolinium-enhanced MRI of brain and orbits. (a) Lesions consistent with demeylination plaques on the left side of the optic chiasm (arrow). (b) Lesions consistent with demyelinating areas in the periventricular region.
• Space occupying lesion (e.g.tumours, aneurysms, arachnoid cysts or hydrocephalus)
• Vasculitis (e.g. systemic lupus erythematosus)
• Inflammation (e.g. sarcoidosis)
• Trauma
• Vitamin B12 deficiency
• Empty sella syndrome
• Pathological myopia
The diagnoses of space occupying lesion and empty sella syndrome were excluded after the initial scans. Our patient did not give a history of trauma and the diagnosis of vitamin B12 deficiency was also excluded as she did not have any symptoms consistent with vitamin B12 deficiency and its serum levels were normal.
Sarcoidosis was not likely to be the cause of the scotoma as chest X-ray did not reveal any relevant signs and angiotensin converting enzyme levels were normal. Pathological myopia was an unlikely diagnosis according to the fundoscopic and intravenous fluorescein angiogram findings.
Vasculitis was a possible diagnosis along with multiple sclerosis. Systemic lupus erythematosus (SLE), albeit rare, is a well established cause of chiasmatis in the international literature.(1,2,3) It can affect the visual pathway by either thrombosis of the visual pathway vasculature or by immunological mechanisms such as vasculitis.(3) Both mechanisms cause ischemia of the affected structures. The differential diagnosis between MS and SLE becomes more confusing by the fact that involvement of the central nervous system by SLE can cause the development of multiple areas of increased signal intensity in the subcortical white matter on T2 weighted images.(1) In addition to that, there is clinical overlap between neurologic manifestations of MS and SLE. Furthermore 81% of patients with MS are positive for antinuclear antibodies (ANA).(2)
In the case of our patient, ANA and anti-double strand DNA antibodies were negative and medical history and systematic examination did not reveal symptoms or signs of SLE. The course of the disease confirms the diagnosis of MS.
The knee of Wilbrand which was initially described by Hermann Wilbrand (8,9) is believed to be made up of crossing fibers that originate from the inferonasal retina (superotemporal visual field), which travel for a short course in the posterior segment of the contralateral optic nerve before they loop back in the contralateral optic tract. As the presence of a RAPD implies an asymmetry of light input between the two eyes, it is likely that the difference in the number of optic nerve fibers affected in the two eyes of our patient was not as great as to clinically produce a RAPD.
The existence of Wilbrand’s knee has been disputed (10) and recent sophisticated studies have not confirmed its presence either in humans or other primates.(11) Despite these findings the junctional scotoma remains a classic example of damage to the optic chiasm.(12,13,14) Neurological and radiological investigations are warranted in a case presenting with junctional scotoma in order to identify the nature of the lesion.
2. Siatkowski RM, Scott IU, Verm AM, Warn AA, Farris BK, Strominger MB, Sklar EM. Optic neuropathy and chiasmopathy in the diagnosis of systemic lupus erythematosus. J Neuroophthalmol. 2001 Sep;21(3):193-8.
3. Giorgi D, Balacco Gabrieli C. Optic neuropathy in systemic lupus erythematosus and antiphospholipid syndrome (APS): clinical features, pathogenesis, review of the literature and proposed ophthalmological criteria for APS diagnosis. Clin Rheumatol. 1999;18(2):124-31.
4. Wilhelm H, Grodd W, Schiefer U, Zrenner E. Uncommon chiasmal lesions: demyelinating disease, vasculitis, and cobalamin deficiency. Ger J Ophthalmol. 1993 Aug;2(4-5):234-40.
5. Frohman LP, Frieman BJ, Wolansky L. Reversible blindness resulting from optic chiasmitis secondary to systemic lupus erythematosus. J Neuroophthalmol. 2001 Mar;21(1):18-21.
6. Tang RA, Grotta JC, Lee KF, Lee YE. Chiasmal syndrome in sarcoidosis. Arch Ophthalmol. 1983 Jul;101(7):1069-73.
7. Milea D, LeHoang P. An unusual junctional scotoma. Surv Ophthalmol. 2002 Nov-Dec;47(6):594-7.
8. Wilbrand H, Saenger A Die Neurologie des Auges. Wiesbaden J Bergmann. 1904; 3(1): 98-120.
9. Wilbrand H. Schema des verlaufs der sehnervenfasem durch das chiasma. Zeitschrift fur Augenheilkunde. 1926; 59: 135-44.
10. Horton J. Wilbrand’s knee of the primate optic chiasm is an artifact of monocular enucleation. Trans Am Ophthalmol Soc. 95:579-609,1997
11. Lee JH, Tobias S, Kwon JT, Sade B, Kosmorsky G. Wilbrand's knee: does it exist? Surg Neurol. 2006 Jul;66(1):11-7; discussion 17.
12. Glaser JS. Neuro-Ophthalmology. Philadelphia. Lippincott, 1990, p78.
13. M Yanoff. Chapter 195 in: Ophthalmology 2nd edition. Mosby. 2004, pp 1290.
14. Kanski. Chapter 18. In: Clinical Ophthalmology: a systematic approach 5th edition. Butterworht – Heinemann. 2003, pp 645 - 646.