A 36-year-old man with a red eye
Digital Journal of Ophthalmology 2008
Volume 14, Number 9
April 13, 2008
Volume 14, Number 9
April 13, 2008
His past medical history was significant for juvenile rheumatoid arthritis and rheumatic fever as a child. He had no drug allergies and his only medications were vicodin and keflex. He denied tobacco or alcohol use and was employed as a prison guard. On review of systems, he had a flu-like illness 10 days prior with fever, myalgias, nausea, vomiting and diarrhea. All of these symptoms had since resolved. He had stable chronic knee pain which was controlled with vicodin. He denied headache, cough, sore throat, shortness of breath, hemoptysis, chest pain, rash, new joint pain, cold sores, genital lesions, dysuria, or mood changes.
Slit lamp examination (see figures 1-3) revealed a scleral shell prosthesis on the left. His eyelids were flat without erythema or swelling bilaterally. His conjunctiva had 3+ injection with ciliary flush on the right and was quiet on the left. There were fine keratic precipitates on the right cornea. The left cornea was opaque due to pannus. There was no view of any deeper structures in the left eye. The right eye had 4+ cell and flare in the anterior chamber, a round and regular iris with no synechiae, and a clear lens. There was vitreous haze in the right eye.
Funduscopic exam of the right eye (see figure 4) showed a normal optic nerve with a cup to disc ratio of 0.3. The vessels were within normal limits, but there were multiple creamy, placoid, deep retinal lesions extending from the right macula to the temporal periphery. There was no view of the left fundus.
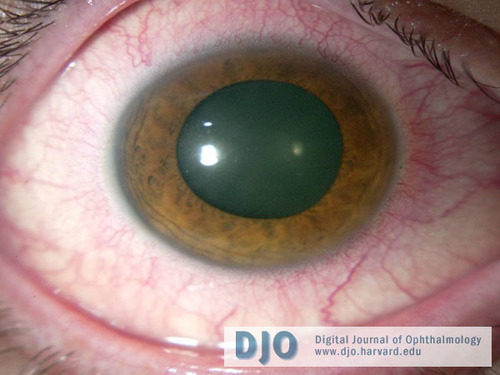
Figure 1
Photograph of the right eye (post-dilation) displaying ciliary flush.
Photograph of the right eye (post-dilation) displaying ciliary flush.
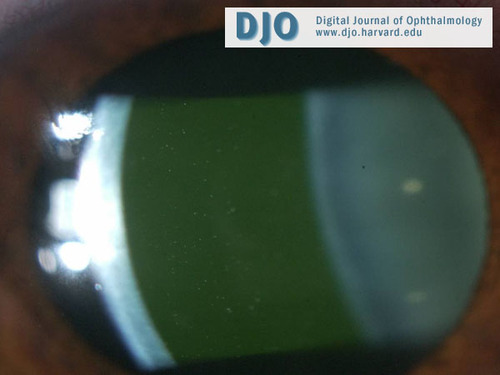
Figure 2
Photograph of the right eye demonstrating anterior chamber cell and flare.
Photograph of the right eye demonstrating anterior chamber cell and flare.
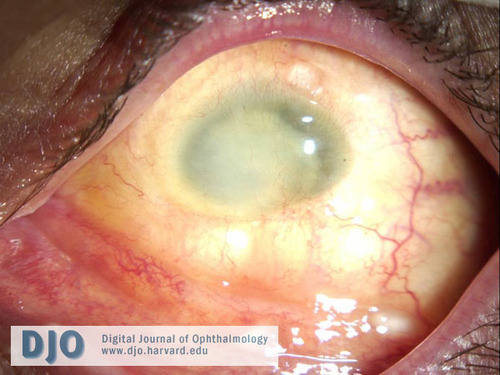
Figure 3
The phthisical left eye after the scleral shell was removed showed no conjunctival injection. According to the patient, he was shot in the left eye 22 years ago. The eye was not removed as there was hope that he would regain vision. However 3 years later when the eye had become phthisical, he was fitted with a scleral shell.
The phthisical left eye after the scleral shell was removed showed no conjunctival injection. According to the patient, he was shot in the left eye 22 years ago. The eye was not removed as there was hope that he would regain vision. However 3 years later when the eye had become phthisical, he was fitted with a scleral shell.

Figure 4
Fundus photo of the right eye demonstrating multiple creamy, placoid, deep retinal lesions in the macula and temporal periphery. The optic nerve and vessels were normal.
Fundus photo of the right eye demonstrating multiple creamy, placoid, deep retinal lesions in the macula and temporal periphery. The optic nerve and vessels were normal.

Figure 5
A red free photo showing placoid lesions of the right fundus.
A red free photo showing placoid lesions of the right fundus.

Figure 6
The arterial phase of the right eye fluorescein angiogram shows early blockage of the lesions.
The arterial phase of the right eye fluorescein angiogram shows early blockage of the lesions.

Figure 7
Venous phase of the right eye fluorescein angiogram.
Venous phase of the right eye fluorescein angiogram.
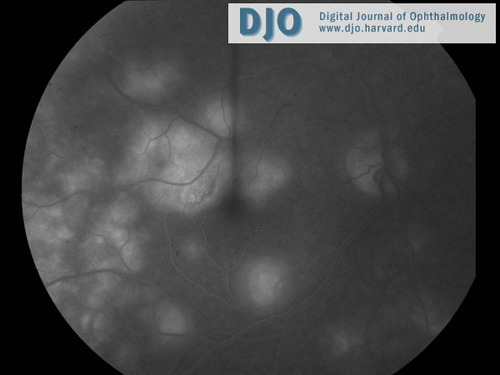
Figure 8
The late phase of the right eye fluorescein angiogram demonstrates late hyperfluorescence of the lesions.
The late phase of the right eye fluorescein angiogram demonstrates late hyperfluorescence of the lesions.
Table 1
Labs and studies that were obtained are listed above with abnormal values in bold.
Labs and studies that were obtained are listed above with abnormal values in bold.
Other than working as a prison guard, our patient gave no other risk factors or history of exposure to any possible infectious cause. He also did not show any systemic signs of illness at the time he was evaluated. Nevertheless, we considered syphilis, tuberculosis, toxoplasmosis, endogenous endophthalmitis, Lyme disease, and toxocariasis as possible infectious causes that needed to be ruled out.
Lastly, we considered neoplastic masquerade syndromes as they constitute 2-3% of all uveitis cases seen at a tertiary uveitis center.(1) Primary CNS lymphoma is the most common cause; however, this neoplasm presents in a much older population than our patient. Leukemia was also unlikely and more commonly presents as a retinopathy. Metastases represents the most common intraocular malignancy in adults and most often presents as choroidal metastases with vitritis,(1) but our patient had no history of a primary tumor.
Sympathetic ophthalmia is a non-necrotizing, granulomatous panuveitis that generally spares the choriocapillaris.(2) The incidence is reported to be 0.2% after accidental trauma and less than 0.1% after surgical trauma.(3) It is theorized that sequestered intraocular antigens gain access to the lymphatic system after a penetrating ocular injury and the predominant cellular infiltrate has been found to be T lymphocytes.(4) Although sympathetic ophthalmia has been found to occur up to 66 years after injury, 65% of cases present between 2-8 weeks after injury and 90% of cases occur within 1 year.(2)
Patients often complain of vision loss, photophobia, and/or pain. Signs can include panuveitis, multifocal infiltrates at the level of the RPE or choroid, thickening of the uveal tract, optic nerve swelling, and/or exudative retinal detachment.
The diagnosis is one of exclusion but is suggested by bilateral uveitis after trauma or injury. Treatment initially consists of corticosteroids (topical, systemic, and/or periocular) and topical cycloplegics or mydriatics. When treated with steroids, the majority of patients retain 20/60 vision or better.(5) Given the long-term need for immunosuppression, a steroid-sparing agent becomes necessary to avoid the dangerous adverse effects of long-term steroid use. There is strong evidence that low-dose cyclosporine (a T-lymphocyte inhibitor) should be considered a first-line immunomodulator with or without concomitant low-dose corticosteroids in cases of chronic non-infectious uveitis (including sympathetic ophthalmia).(6) Mycophenolate mofetil is a newer immunomodulator with a better side effect profile. There is moderate evidence of efficacy showing that mycophenolate mofetil should be used for chronic non-infectious uveitis when other immunosuppressive drugs have failed or have not been tolerated.(7) Alkylating agents (i.e. chlorambucil or cyclophosphamide) and antimetabolites (i.e. azathioprine) or a combination of two immunosuppressive agents may also be considered in patients with resistant vision-threatening inflammation.(7)
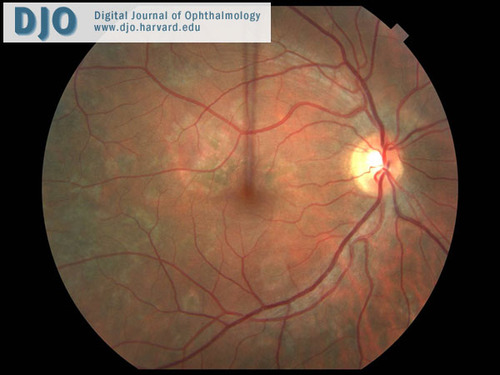
Figure 9
A right eye fundus photo shows fading of the choroidal lesions after 2 weeks of treatment.
A right eye fundus photo shows fading of the choroidal lesions after 2 weeks of treatment.
2. Boyd SR, Young S, Lightman S. Immunopathology of the Noninfectious Posterior and Intermediate Uveitides. Survey of Ophthalmology. 2001; 46(3): 209-233.
3. Kilmartin DJ, Dick AD, Forrester JV. Prospective Surveillance of Sympathetic Ophthalmia in the UK and Republic of Ireland. British Journal of Ophthalmology. 2000; 84: 259-263.
4. D’Amico FM, Kiss S, Young LH. Sympathetic Ophthalmia. Seminars in Ophthalmology. 2005; 20(3): 191-197.
5. Chu D, Foster CS. Sympathetic Ophthalmia. International Ophthalmology Clinics. 2002; 42(3): 179-185.
6. Jabs DA, Rosenbaum JT, Foster CS, et al. Guidelines for the Use of mmunosuppressive Drugs in Patients with Ocular Inflammatory isorders. American Journal of Ophthalmology. 2000; 130(4): 492-513.
7. Okada AA. Immunomodulatory Therapy for Ocular Inflammatory Disease. Ocular Immunology and Inflammation. 2005; 13:335-351.