A 39-year-old man with painful proptosis after dental extraction
Digital Journal of Ophthalmology 2008
Volume 14, Number 4
February 7, 2008
Volume 14, Number 4
February 7, 2008

Figure 1
External photograph demonstrating left proptosis, periorbital edema, and chemosis
External photograph demonstrating left proptosis, periorbital edema, and chemosis
Computed tomography of the head was performed, revealing opacification of the left anterior ethmoid and maxillary sinuses. In addition, an intraconal collection of fluid with an adjacent gas bubble was identified lateral to the optic nerve, exerting mass effect on the posterolateral aspect of the globe.
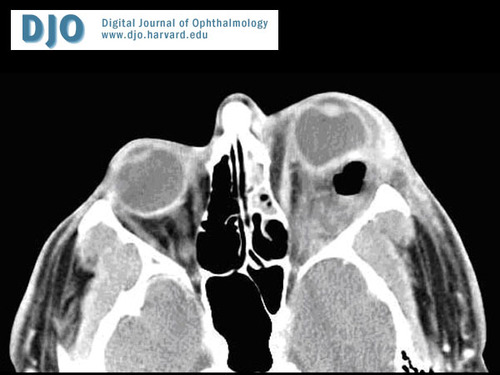
Figure 2
Axial CT image demonstrating intraconal gas with posterolateral globe deformation.
Axial CT image demonstrating intraconal gas with posterolateral globe deformation.

Figure 3
Coronal CT image
Coronal CT image
Microbiologic cultures obtained intraoperatively revealed growth of group F Streptococcus, coagulase negative Staphylococcus, and mixed anaerobic flora.
Four days after surgical intervention, the patient’s visual acuity in the left eye was 20/30, no afferent pupillary defect was evident, the periorbital edema and proptosis had significantly improved, and motility was nearly full.

Figure 4
Intraoperative photograph demonstrating a purulent orbital fluid collection with surfacing gas bubbles.
Intraoperative photograph demonstrating a purulent orbital fluid collection with surfacing gas bubbles.
Intraorbital gas due to an infectious agent is an uncommon finding(2,3) and indicates the need for prompt surgical intervention and/or treatment with broad-spectrum antimicrobial agents. Anaerobic organisms must be considered when choosing an antibiotic in these cases. The patient presented here had undergone a dental extraction, which has been associated with transient bacteremia, including anaerobic species.(4) The possibility of hematogenous spread cannot be ruled out as the orbital collection in this case was posterolateral to the globe and direct intraorbital extension of an infectious sinus process is more frequently medially located. In patients with this clinical picture, further investigation for other sites of bacteremic seeding may be warranted.
Atypical organisms are potential offending infectious agents in immunocompromised individuals.(1) There should also be high suspicion for fungal infections in this patient population. This patient had been treated with oral steroids without antibiotics for 5 days prior to presentation and this may have contributed to the development of gas-producing bacteria.
The formation of gas has most commonly been linked to Clostridium perferingens, but other bacteria including Staphylococci, Streptococci, and other anaerobes have been shown to be capable of causing gas-forming infections.(5) Initial antibiotic treatment should be guided by the results of Gram stain and deliberation of possible etiologic agents based on clinical findings. The excellent outcome in the patient presented here can be attributed in part to prompt and aggressive treatment.
2. Rose GE, Hadley J, Morgan D, Thompson P. Acute orbital cellulitis due to gas-forming bacteria. Eye. 1991; 5 (5):640-1.
3. Zimmer-Galler IE, Bartley GB. Orbital emphysema: case reports and review of the literature. Mayo Clin Proc. 1994; 69(2):115-21.
4. Rajasuo A, Perkki K, Nyfors S, Jousimies-Somer H, Meurman JH. Bacteremia Following Surgical Dental Extraction with an Emphasis on Anaerobic Strains. J Dent Res. 2004; 83(2): 170-4.
5. Bessman AN, Wagner W. Non-clostridial gas gangrene. JAMA. 1975;233:958-63.