A 37-year-old woman with spontaneous lens dislocation after vitrectomy for retinal reattachment
Digital Journal of Ophthalmology 2008
Volume 14, Number 5
February 10, 2008
Volume 14, Number 5
February 10, 2008
Two weeks later, the visual acuity was hand movements in the right eye. The lens had dislocated to the inferior vitreous cavity, with recurrence of the retinal detachment (figure 1).
The patient underwent repeat vitrectomy, lensectomy to remove the dislocated lens, cryotherapy to a dialysis at 6 o’clock and 16% C3F8 gas tamponade. On the first postoperative day visual acuity was hand movements, there was moderate corneal edema and 80% fill of the vitreous cavity with gas.
Two months post-operatively the best corrected visual acuity is 6/12 in the right eye with aphakic correction. The plan for the patient is to perform a secondary intraocular lens implantation. There was no lens instability of the fellow eye during the whole period that the patient was under our care.
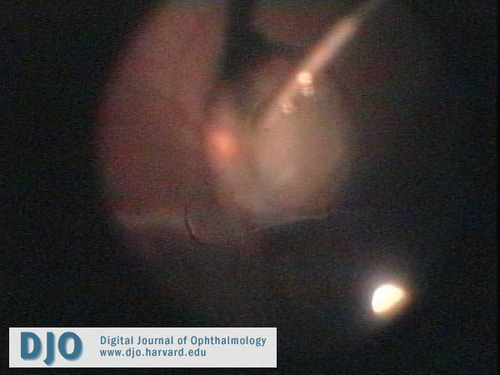
Figure 1
Lensectomy of the crystalline lens dislocated into the vitreous cavity
Lensectomy of the crystalline lens dislocated into the vitreous cavity
Well-known conditions that are associated with fibrillin disruption are Marfan syndrome and ectopia lentis and both may present with lens dislocation.(1) Previous reports have highlighted on surgery for subluxed/dislocated lens in Marfan patients.(2,3) There is also reference in literature about retinal re-attachment surgery in such patients.(4) Spontaneous lens dislocation has been reported in pseudoexfoliation(5), uveitis(6) and following scleral buckling procedure.(7, 8)
In our patient the causes for the spontaneous dislocation of the lens could be attributed to either a subclinical zonular weakness related to Marfan or due to peri-operative imperceptible zonular damage during vitrectomy and subsequent gas pressure on the lens. Surgery for retinal re-attachment has been associated with many postoperative complications. To the best of our knowledge spontaneous dislocation of lens following vitrectomy is a very rare complication.
2. Omulecki W, latecka-Krajewaska B, Palenga-Pydyn D et al.( treatment of dislocated lenses in patients with Marfan’s syndrome using vitrectomy and intraocular lenses) ( Article in Polish) Klin Oczna. 2002; 104(1): 19-22.
3. Vadala P, capozzi P, Fortunato M et al. Intraocular lens implantation in Marfan’s syndrome. J Pediatr Ophthalmol strabismus. 2000; 37(4):206-8.
4. Sharma T, Gopal L, Shanmugam MP et al. Retinal detachment in Marfan’s syndrome: clinical character and surgical outcome. Retina. 2002 Aug;22(4): 423-8.
5. Tyagi AK, McDonnell PJ. Pseudoexfoliation syndrome and spontaneous lens dislocation. Eye. 1998; 12(6):1033-4.
6. Belfort R Jr, Nussenblatt RB, Lottemberg C et al. Spontaneous lens subluxation in uveitis. Am J Ophthalmol. 1995 Dec 15; 110(6):714-6.
7. Tornambe P, Hilton G. The retinal detachment study group Pneumatic retinopexy. A multicenter randomised controlled clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology. 1989; 96:772-884.
8. Sullivan P, Luff A, Aylward G. Results of primary retinal reattachment surgery: A prospective audit. Eye. 1997; 11: 869-871.