A 38-year-old man with bilateral foveal hemorrhages
Digital Journal of Ophthalmology 2008
Volume 14, Number 7
March 11, 2008
Volume 14, Number 7
March 11, 2008
There was no significant past medical history; specifically, there was no history of diabetes or hypertension.
The anterior segment examination was normal.
Dilated fundoscopic examination showed bilateral foveal preretinal hemorrhages and bilateral scattered nerve fiber layer hemorrhages. The foveal hemorrhages were beginning to organize at the time of presentation to our department.
Blood pressure, blood glucose and complete blood count were normal. Specifically, there was no evidence of anemia.
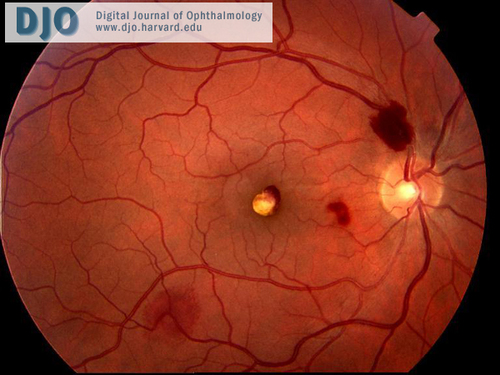
Right eye
Fundus photograph demonstrating foveal pre-retinal hemorrhage and scattered nerve fiber layer hemorrhages.
Fundus photograph demonstrating foveal pre-retinal hemorrhage and scattered nerve fiber layer hemorrhages.
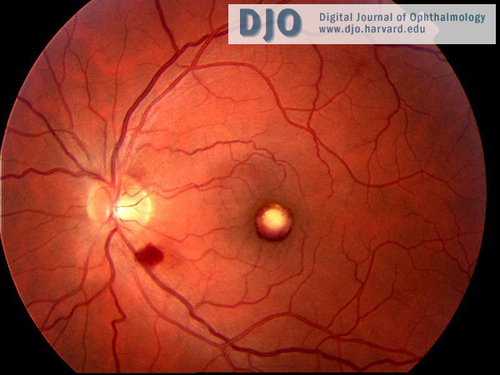
Left eye
Fundus photograph demonstrating organizing foveal pre-retinal hemorrhage and a nerve fiber layer hemorrhage in the inferior arcade.
Fundus photograph demonstrating organizing foveal pre-retinal hemorrhage and a nerve fiber layer hemorrhage in the inferior arcade.
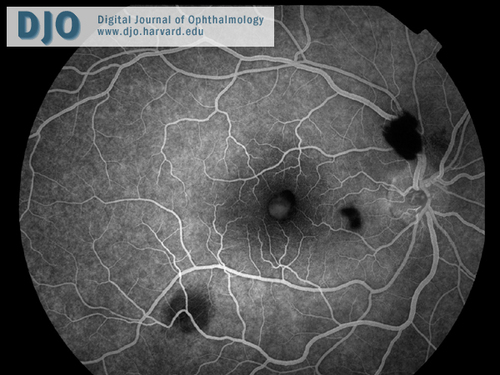
Fluorescien angiogram right eye

Fluorescien angiogram left eye
• Diabetic retinopathy- The patient in this case did not have diabetes.
• Hypertensive retinopathy- The patient in this case did not have hypertension.
• Central retinal vein occlusion- The fluorescein angiographic appearance shows no evidence of venous occlusion.
• Purtscher's retinopathy- Classically associated with chest trauma, this condition may also be seen in association with pregnancy, fat embolism and pancreatitis. None of these are relevant in this case.
• Leukemic retinopathy- Leukemias, in particular myeloid leukemia, may be associated with retinopathy. Features of leukemic retinopathy include preretinal and intraretinal haemorrhages. Other features include Roth’s spots, cotton wool spots, retinal venous tortuosity and neovascularization. There was no other evidence of leukemia in this case.
• Valsalva retinopathy- This will be discussed further in the Diagnosis and Discussion section.
• High-Altitude Retinopathy- This will be discussed further in the Diagnosis and Discussion section.
A number of factors are thought to contribute to the pathophysiology of the condition including increased retinal blood flow associated with reduced arterial oxygen pressures, reduced vascular competence (2) and inadequate autoregulation of the retinal circulation in hypoxic conditions.(3) It has also been found to be more common in those with higher baseline intraocular pressures and those who have used non-steroidal anti-inflammatory drugs.(2)
The Valsalva maneuver (forcible exhalation against a closed glottis) can be associated with a retinopathy characterized by rupture of perifoveal capillaries and unilateral or bilateral pre-macular hemorrhages. It has been suggested that this maneuver contributes to the pathophysiology of HAR but the intraretinal hemorrhage, retinal venous dilation and optic disc edema which may be seen in HAR are not features of Valsalva retinopathy.(4)
HAR has a benign course and usually is associated with good long-term visual outcomes. However, high altitude retinopathy is part of a spectrum of life threatening conditions which constitute altitude sickness. These conditions are acute mountain sickness (AMS), high-altitude retinopathy, high-altitude cerebral edema (HACE) and high-altitude pulmonary edema (HAPE). High-altitude retinopathy is associated with HACE. The presence of retinopathy findings in climbers should alert physicians to the possibility of cerebral edema.(1)
Treatment for HAR alone is rarely required but treatment of the systemic altitude sickness may include descent, administration of oxygen, steroids or diuretics.(1)
2. Butler FK, Harris DJ, Reynolds RD. Altitude Retinopathy on Mount Everest, 1989. Ophthalmology. 1992; 99(5) 739-746
3. Mullner-Eidenbrock A, Rainer G, Strenn K, Zidek T. High-altitude retinopathy and retinal vascular dysregulation. Eye. 2000; 14(5): 724-729
4. Duane TD. Valsalva hemorrhagic retinopathy. Transactions of the American Ophthalmological Society. 1972; 70: 298-313.